Seborrheic Dermatitis on the Scalp & Face
Seborrheic dermatitis is one of the most common skin conditions, characterized by flaking skin, greasy patches with white or yellow scales or crust, itchiness, and rash, affecting between 3 and 5% of the general population. This common dermatologic issue typically impacts the scalp but can also affect areas with a high concentration of sebaceous glands, which produce excess oil (sebum). These areas include the face, sides of the nose, ears, chest, eyelids, and eyebrows. While seborrheic dermatitis is not dangerous or a sign of more serious health problems, many patients find it uncomfortable and frustrating or may feel self-conscious about dandruff and flare-ups. Fortunately, many treatment options are available at board-certified dermatologist Dr. Michele Green’s New York City dermatology office.
For some patients, seborrheic dermatitis may clear up without the need to visit a healthcare provider. For others, it might persist without treatment. In those cases, the best first step is to schedule an appointment with an experienced dermatologist, such as Dr. Green. Depending on the severity of the condition, Dr. Green may recommend topical antifungal lotions, prescription medicated shampoos, over-the-counter dandruff shampoos, topical corticosteroids, topical calcineurin inhibitors, or phototherapy. She may also provide guidance on skincare routines or lifestyle changes that could help reduce future flare-ups. To find the best treatment option for you, schedule an initial consultation with Dr. Michele Green.
Experienced, board-certified dermatologist Dr. Michele Green has been expertly treating patients at her Upper East Side, New York City, office for over 25 years. A master of various cosmetic and medical skincare treatments, Dr. Green is highly skilled at creating personalized, effective skincare plans tailored to each patient. With her proprietary line of skincare products, MGSKINLABs, Dr. Green can offer patients personalized recommendations for the highest-quality creams, lotions, and serums. Renowned for high patient satisfaction, Dr. Green has been named one of the best dermatologists in New York City by publications such as Castle Connolly, Super Doctors, and New York Magazine.

What is Seborrheic Dermatitis?
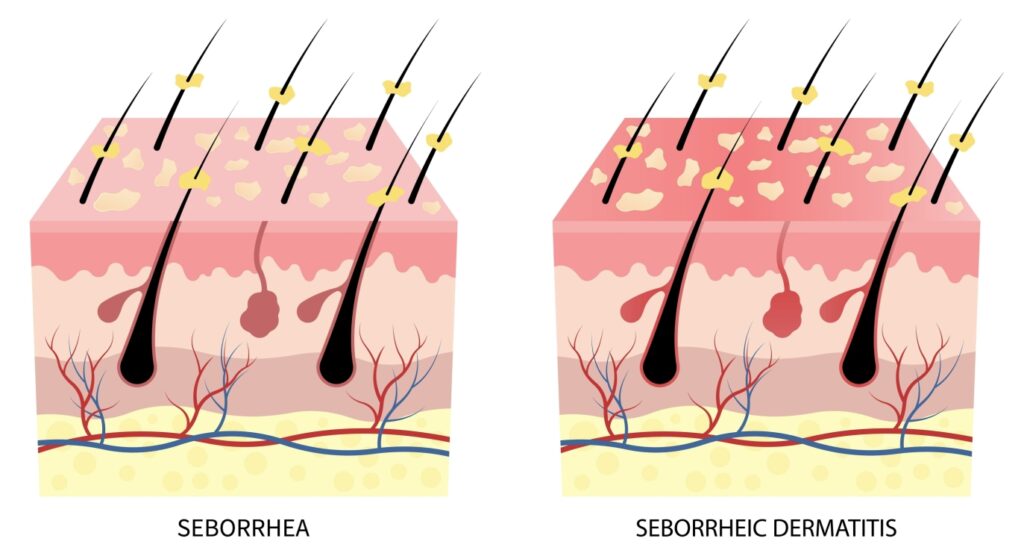
Seborrheic dermatitis is a common skin condition that most often affects areas of the body prone to oily skin, such as the scalp, face (sides of the nose, beard, eyelids, eyebrows), chest, armpits, groin area, and other skin folds and creases. Specifically, it occurs in areas with high concentrations of sebaceous glands and excess oil production. It is more common in men than women and affects patients with darker skin at a higher rate than those with lighter skin. Seborrheic dermatitis is characterized by flaking skin—also known as dandruff—greasy patches with white or yellow scales, redness caused by irritation and inflammation, and crusted-over lesions. While it isn’t a dangerous or contagious condition, it can be very uncomfortable in the affected areas. Because of its visibility on the face and scalp, some patients may feel self-conscious. Fortunately, many treatment options are available at Dr. Green’s New York City dermatology office.
Why do I have Seborrheic Dermatitis?
Although the exact cause of seborrheic dermatitis is still unknown, several factors may contribute to its development. Researchers suggest that a buildup of the malassezia yeast (sometimes called pityrosporum) that grows on areas of the body with high oil production could be partly responsible. Malassezia yeast feeds on excess skin oil, transforming it into fatty acids that irritate the skin, causing redness, itching, and flaking. This skin irritation further worsens seborrheic dermatitis as the skin barrier weakens, reducing the skin’s ability to retain moisture. This leads to increased oil production, which feeds the malassezia yeast even more. Another possible factor is an underlying immunodeficiency or a weakened immune system. Regardless of the exact cause, seborrheic dermatitis can be a lifelong condition, with periodic flare-ups.
What are the risk factors for developing seborrheic dermatitis on the scalp?
While the exact cause of seborrheic dermatitis is still unknown, several risk factors can contribute to flare-ups and the initial development of the condition. These factors include:
- Stress or recovery from a stressful medical condition
- Fatigue
- Genetics or a family history of the skin condition
- Changes in seasons or exposure to cold, dry weather
- Contact with harsh chemicals, such as cleaning supplies or paint
- Use of harsh, alcohol-based skincare products
- Health conditions affecting the nervous system, like epilepsy or Parkinson’s Disease
- Mental health issues, such as depression or anxiety
- Other skin conditions, such as psoriasis or rosacea
- Immune system disorders, such as HIV
Not all individuals with these factors will develop seborrheic dermatitis, but they can increase the risk of flare-ups and exacerbate a pre-existing condition.
Is seborrheic dermatitis dandruff?
Seborrheic dermatitis is a common skin condition also known as dandruff, seborrheic psoriasis, or seborrheic eczema. It can affect people of any age but is most common in adolescents and those between 30 and 60 years old. When it affects infants, it is often called “Cradle Cap.” In addition to developing seborrheic dermatitis on the scalp, infants can also experience the condition on their bottoms, chests, backs, and between skin folds.
How to treat seborrheic dermatitis
Patients often wonder, “How do you get rid of seborrheic dermatitis?” While seborrheic dermatitis cannot be completely cured, various treatment options are available to relieve symptoms and prevent future flare-ups. The best first step is to schedule a consultation with a board-certified dermatologist, such as Dr. Michele Green. During the appointment, Dr. Green will examine the affected area. Depending on the severity, she may perform a skin biopsy to confirm if seborrheic dermatitis is the cause of the irritation. After your diagnosis, Dr. Green will recommend the most suitable treatment options, which may include over-the-counter dandruff shampoos, prescription topical antifungal lotions, prescription shampoos, corticosteroids, or phototherapy. Depending on the severity and chosen treatment, you might need to continue these products long-term to prevent flare-ups. Make sure to follow Dr. Green’s instructions to avoid unwanted side effects.
How to treat seborrheic dermatitis on the scalp
Seborrheic dermatitis most commonly affects the scalp, causing scaly, flaky, greasy patches of skin that are often red and irritated. It can also lead to dandruff, characterized by dry, flaky skin that frequently falls onto the shoulders. To start treating seborrheic dermatitis on the scalp, Dr. Green usually recommends an over-the-counter dandruff shampoo with ingredients like zinc pyrithione, selenium sulfide, or coal tar. These products are typically best for mild cases. For patients needing a stronger solution, Dr. Green may prescribe an antifungal shampoo containing ingredients such as ciclopirox or ketoconazole. According to an article published in the Journal of the American Academy of Dermatology (J Am Acad Dermatol), ketoconazole shampoo is very effective at reducing dandruff, itching, and irritation in patients with moderate to severe seborrheic dermatitis (DOI: 10.1016/0190-9622(93)70282-X). Some patients with severe seborrheic dermatitis might benefit from shampoos with steroids like clobetasol, fluocinolone, or betamethasone valerate. After your initial consultation, Dr. Green will give instructions on how often to use these shampoos and for how long.

How to treat seborrheic dermatitis on the face
In addition to appearing on the scalp, seborrheic dermatitis can also affect areas of the face, including the eyebrows, eyelids, sides of the nose, and beard. To treat affected areas on the face, Dr. Green may suggest using topical antifungal products, such as lotions containing clotrimazole and ketoconazole, to help reduce the amount of Malassezia yeast. Some topical corticosteroids, like hydrocortisone, can also help control seborrheic dermatitis flare-ups by decreasing inflammation and redness. Topical calcineurin inhibitors, such as pimecrolimus cream or tacrolimus ointment, can be a good alternative to corticosteroids. Additionally, some oral antifungal medications, including itraconazole, terbinafine, and fluconazole, may also help lessen the appearance of seborrheic dermatitis on the face. In-office treatments, such as phototherapy, can also be effective when performed by an experienced dermatologist, like Dr. Green.
How to treat cradle cap
Cradle cap is the term used for cases of seborrheic dermatitis that affect infants, most commonly appearing on the scalp. However, cradle cap can also occur on other parts of the body, including the bottom, back, chest, skin folds, and face. When treating cradle cap, dandruff shampoos are not recommended for infants and should not be used on the face or eyebrows. Instead, Dr. Green suggests applying petroleum jelly, such as Vaseline or Aquaphor, to gently loosen the flakes in the affected areas. Parents can also wash the area more often with care, avoiding scratching or picking at the scales.
How to treat seborrheic dermatitis naturally
Patients often ask, “How can I treat scalp dermatitis naturally?” The best way to manage seborrheic dermatitis is to consult a board-certified dermatologist, such as Dr. Green. If you’re interested in treatments with more natural ingredients, Dr. Green can recommend products containing tea tree oil or salicylic acid. Additionally, patients can modify their lifestyle habits and skincare routines to lower the risk of a seborrheic dermatitis flare-up. By reducing stress, getting enough sleep, and keeping skin clean and moisturized, patients are less likely to experience flare-ups. Some “natural” products, like coconut oil, may worsen skin conditions, so it’s important to consult with a dermatologist first.
How to stop seborrheic dermatitis
Seborrheic dermatitis is not a dangerous skin condition and does not indicate any underlying health issues. Some patients may control their condition through lifestyle changes—such as reducing stress, getting enough sleep, and improving their skincare routine—while others may find that their symptoms do not improve on their own. Dr. Green recommends scheduling an appointment to address seborrheic dermatitis if the condition becomes so uncomfortable that it disrupts sleep or daily activities, if lifestyle changes have had no effect, or if the condition makes you feel self-conscious. After your initial consultation with Dr. Green, she will suggest treatment options that are likely to be most effective for you, which may include prescription shampoos, antifungal lotions, corticosteroids, or in-office treatments.

Can seborrheic dermatitis cause hair loss?
Seborrheic dermatitis does not lead to permanent hair loss. Scratching, itching, and flaking on the scalp can cause some hair shedding, but hair should grow back once the underlying condition is treated. If left untreated, severe seborrheic dermatitis can irritate the scalp, damage hair follicles, and potentially cause more permanent hair loss.
What is the best shampoo for seborrheic dermatitis?
Medicated shampoos are very effective at reducing seborrheic dermatitis symptoms and preventing future flare-ups. Most dandruff shampoos should be left on the scalp for at least five minutes before washing off, which can also help treat seborrheic dermatitis on the body. The best shampoo for seborrheic dermatitis depends on the severity and location of your condition. During your consultation, Dr. Green will help you find the most suitable treatment. Generally, the most effective shampoos for seborrheic dermatitis contain ingredients such as:
- Zinc pyrithione
- Selenium sulfide
- Ketoconazole
- Coal tar
- Tea tree oil
- Salicylic acid
Does coconut oil help seborrheic dermatitis?
Coconut oil on the scalp has been promoted as an effective treatment for seborrheic dermatitis. However, it can actually worsen the condition when used on the scalp. Although coconut oil has antifungal properties, it contains fatty acids that feed malassezia yeast, which causes seborrheic dermatitis. The best natural ways to treat seborrheic dermatitis are to reduce stress, get enough sleep, and keep the skin clean and moisturized.
How to help eczema on the scalp
Patients often wonder, “How can I fix eczema on the scalp?” Seborrheic eczema is another term for seborrheic dermatitis, which is characterized by redness, irritation, and inflammation of the skin. To reduce the appearance of eczema on the scalp, Dr. Green frequently recommends patients use medicated shampoos, topical antifungal lotions, or in-office treatments such as phototherapy. It is vital to follow your dermatologist’s instructions to minimize skin irritation and prevent future flare-ups of the condition.
How did I get seborrheic dermatitis?
Seborrheic dermatitis is a common skin condition that affects about 3-5% of the general population. Although researchers don’t yet understand the exact cause, it is not contagious and cannot be transmitted to others. People with a family history of the condition, weakened immune systems, or certain medical issues may be at higher risk of developing seborrheic dermatitis. Since it is a chronic condition, it cannot be completely cured. However, patients can control the symptoms using medicated shampoo, topical antifungal treatments, and a consistent skincare routine.
Which of the following is a form of seborrheic dermatitis:
Contact Dermatitis
Contact dermatitis is marked by skin irritation or an allergic reaction that occurs when certain materials touch the skin, causing discomfort, itching, redness, and swelling. Patients can experience two types of contact dermatitis: allergic contact dermatitis, which usually develops over time when the skin contacts an allergen such as metal jewelry, fragrances, or makeup products; or irritant contact dermatitis, which occurs immediately after exposure to irritants like chemical cleaning products, soaps, or acids. Contact dermatitis is different from seborrheic dermatitis, which is not caused by an allergic reaction.
Atopic Dermatitis
Atopic dermatitis (eczema) is a genetic skin condition characterized by a weakened skin barrier that cannot retain moisture, leading to cracked, dry, irritated, sensitive, bumpy, or blistered skin. Eczema rash can also result from an overgrowth of the bacteria Staphylococcus aureus on the skin’s surface, which can further weaken the skin barrier and disrupt other bacteria. When the skin barrier is compromised, the immune system may trigger inflammation, causing a rash to form. Seborrheic dermatitis is a type of atopic dermatitis, likely caused by the skin’s reaction to the Malassezia yeast.
Seborrheic Keratosis
Seborrheic keratosis is a common skin condition marked by oval-shaped, waxy skin spots that develop over time. Mostly affecting people over 50, seborrheic keratoses are harmless skin growths, meaning they are noncancerous and not dangerous. Typically, these growths are light tan, brown, or black, and they usually appear on the face, neck, chest, or back. While seborrheic keratoses can look warty, they are different from warts because a virus or bacteria cause warts, whereas seborrheic keratoses are not.
Seborrheic keratosis is not the same as seborrheic dermatitis—they are two distinct skin conditions that require different diagnoses and treatments. While seborrheic keratoses are characterized by small, scaly wart-like lesions most commonly found on the face, neck, back, and chest, seborrheic dermatitis typically affects the scalp or other greasy areas of the face, like the eyebrows, beard, armpits, or mustache.

How to treat seborrheic dermatitis today
Seborrheic dermatitis is a common skin condition characterized by flaking, scaly skin, greasy patches, and crusted lesions that cause redness, swelling, and irritation. Also known as dandruff, seborrheic eczema, or seborrheic psoriasis, it is not a dangerous condition, but it can be itchy, irritating, and make patients self-conscious. Fortunately, many treatment options are available at the office of board-certified dermatologist Dr. Michele Green. After assessing the extent and severity of your condition, Dr. Green can recommend and prescribe medicated shampoos, topical antifungal lotions, oral antifungal medications, corticosteroids, or in-office procedures like phototherapy. To determine which treatment options will work best for you, schedule an initial consultation with Dr. Green.
Dr. Michele Green is a highly regarded, board-certified dermatologist with over 25 years of experience offering the best non-invasive treatments. She adopts a holistic, less-is-more philosophy and develops personalized skincare routines and treatment plans tailored to her patients’ unique concerns and aesthetic goals. Recognized consistently as one of New York’s top dermatologists by Castle Connolly, New York Magazine, and Super Doctors, she is known for her dedication and expertise. Please call us at 212-535-3088 or email our New York City-based office today to schedule a consultation with Dr.
 212-535-3088
212-535-3088