Keloid Scar Treatment
Keloid scars are raised, thick scars that develop as part of the body’s natural healing process in response to an injury, infection, burn, or inflammation. These scars form due to excess collagen produced during healing and continue to grow beyond the limits of the initial trauma even after the skin has healed. While scarring is natural, keloid scars can be painful, itchy, and uncomfortable, negatively impacting a person’s self-esteem and confidence. Unlike other types of scars, keloid scars do not fade on their own and require intervention. Fortunately, Dr. Michele Green in New York City is an expert in improving the appearance of keloid scars.
There are various non-surgical and surgical options available for treating keloid scars. Corticosteroid injections, cryotherapy, and radiotherapy can flatten and shrink these scars. Pulsed-dye lasers, such as the VBeam laser, effectively reduce the red pigmentation of the scar, thus improving its discoloration. In some cases, surgical excision may also be recommended. After treatment or injury, silicone gel sheets and pressure garments are used to prevent the formation of new keloids. Keloid scar treatments typically require multiple sessions and are often combined for optimal cosmetic results. Given the high recurrence rates after keloid scar treatments, it is crucial to consult an expert like Dr. Green, who will develop a combination treatment strategy for your keloid scars, helping you achieve clear, radiant skin.
Dr. Michele Green is a world-renowned, board-certified dermatologist with over two and a half decades of experience providing some of the world’s most discerning individuals with the finest non-invasive cosmetic procedures, including VBeam laser treatment and intralesional corticosteroid injections for keloid scars. She is consistently ranked among New York’s top dermatologists by Super Doctors, Castle Connolly, and New York Magazine, thanks to her expertise and dedication to her patients. When you consult with Dr. Green at her private dermatology office in Manhattan’s Upper East Side regarding keloid scar treatment, she will work with you to develop a customized scar treatment plan tailored to your skin type, the location and size of the scar, and your overall aesthetic goals.
Why do hypertrophic scars form?
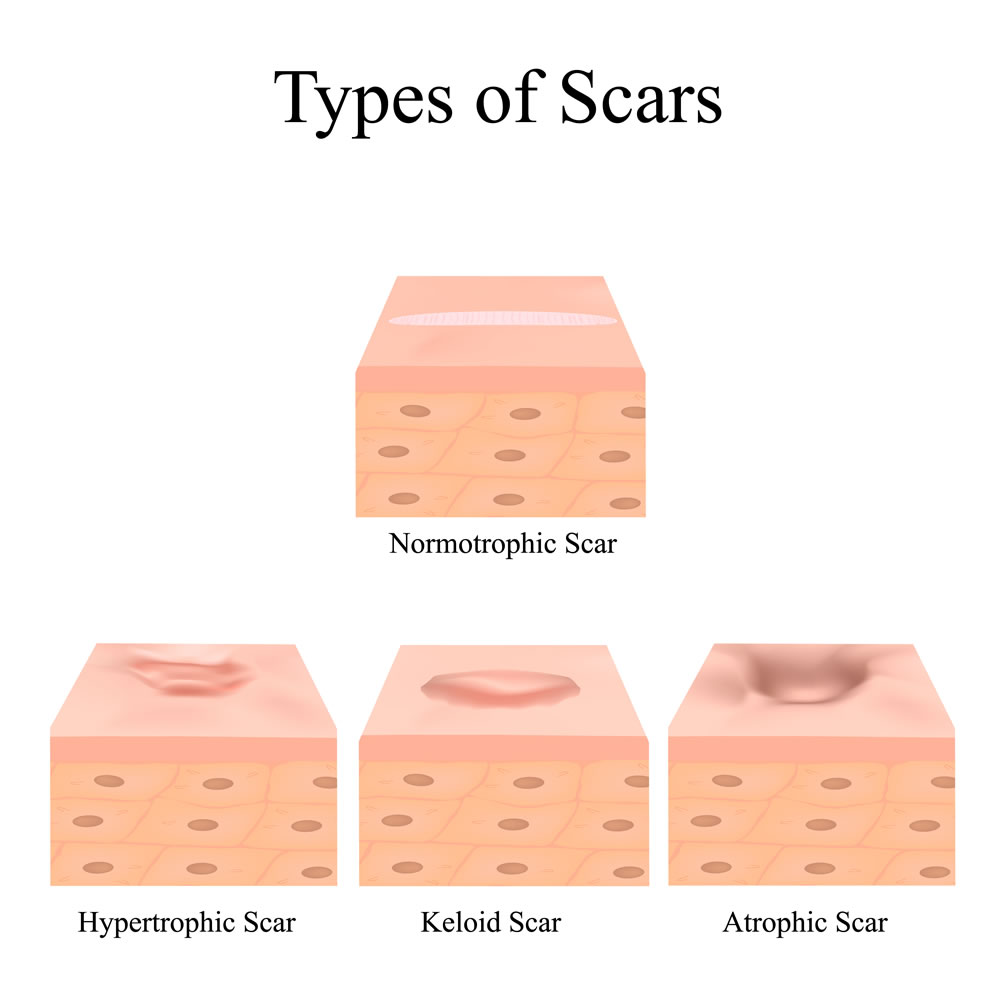
Scars form during the healing process as a result of the body’s natural response to an inflicted wound. Various types of scars can develop from different adverse events, leading to the appearance of multiple scars. Hypertrophic scars occur when fibroblasts in the skin become overactive, producing excess collagen and resulting in a raised scar. While hypertrophic scars may fade over time, they will never completely flatten. These scars do not extend beyond the area of the initial injury. Keloid scars, however, are similar to hypertrophic scars but continue to grow beyond the boundary of the original injury. Scars can form on any part of the body, and the type of scar primarily depends on the nature of the injury or lesion, how the body heals, and the characteristics of the wound.
What is keloid scarring?
A keloid is a type of hypertrophic scar that is firm, raised, and resembles a growth. A hypertrophic scar is a thick, raised scar resulting from an excessive amount of collagen produced during the healing process. Collagen, a structural skin protein, contributes to a firm foundation and an overall youthful appearance. Unlike typical hypertrophic scars, keloids can continue to grow after the skin trauma has healed, extending beyond the borders of the original wound. Keloids may form in response to surgical incisions, piercings, tattooing, insect bites, burns, lacerations, abrasions, vaccinations, chickenpox, and various skin conditions resulting in inflammation or trauma. If a different skin condition appears to have caused the keloid, a skin biopsy may be performed for a definitive diagnosis. The color of keloid scars can vary and may change over time as the scar develops; they may be flesh-colored, red, or hyperpigmented. While keloids are benign growths, they can cause discomfort through sensations of burning, itching, or pain in the affected area. Keloids can develop on any part of the body but are most commonly found on the chest, shoulders, cheeks, and earlobes. Keloids do not resolve on their own and require intervention to treat. They can be a particularly challenging type of scar to manage, and successfully reducing them necessitates treatment by a plastic surgeon or a board-certified dermatologist, such as Dr. Michele Green in New York City.
Are keloid scars hereditary?
While anyone can develop keloid scars after an injury, some individuals are more prone to them. The causes of keloids are still being researched, but certain risk factors have been identified. A significant risk factor for keloid scar formation is having a family history of keloids, as current research indicates a genetic component. Individuals with darker skin tones, such as those of African, Asian, and Hispanic descent, develop keloid scars at a higher rate compared to those with lighter skin tones. Those who have previously experienced keloids or have wounds that take longer to heal are also at higher risk of developing keloid scars. Surgeries involving mesh skin grafts, which help transfer healthy skin from one part of the body to another, can increase the likelihood of developing keloid scars. Lastly, events such as puberty or pregnancy may lead to an increased risk of keloid scars, as hormonal changes during these periods can affect wound healing processes.
How do you prevent a keloid scar from forming?
A common question asked in Dr. Green’s boutique dermatology office is, “How to stop a keloid from forming?” Patients with a history of keloid scars should avoid injuries and trauma to the skin that could lead to scarring. Once an injury occurs, they should follow proper wound care by cleaning the wound and covering it with Aquaphor and a bandage until it has healed completely. The bandage and Aquaphor should be changed daily. The scar must be protected from UV radiation, as ultraviolet light from the sun can darken scars and slow healing. Therefore, a broad-spectrum SPF 30+ should be used consistently to shield the scar. Finally, silicone scar sheets can help prevent keloids from forming and may reduce the size of existing scars.

How to treat keloid scars:
Topical treatments
Silicone gel sheets are a common topical treatment for keloid scars. These medical-grade silicone scar sheets can be used on recent wounds or new keloids to prevent raised scars from forming and to help flatten existing keloids. Researchers have found that while silicone ointment is also available, silicone sheets are more effective at preventing scarring. Silicone gel sheets should never be applied to an open wound or a scab; once the wound has healed, the silicone gel sheets can then be applied. In some cases, a dermatologist may recommend using silicone sheets after treatments like keloid surgery to prevent keloids from reforming.
A pressure garment can also be applied after keloid treatment to reduce the risk of recurrence. By applying constant pressure to the site, pressure garments limit the amount of scar tissue formed during the healing process, thus preventing keloid formation. These garments are often used following treatments such as cortisone injections and keloid surgery. Additionally, pressure earrings are available to treat keloids on the earlobe that result from an ear piercing.
Intralesional injections (Corticosteroids, Bleomycin, 5-fluorouracil)
Intralesional corticosteroid injections are a popular in-office treatment option for reducing the appearance of hypertrophic or keloid scars. Corticosteroids are synthetic drugs that mimic hormones naturally found in the body. Triamcinolone is the most commonly used steroid in injections for keloids. The corticosteroids are injected directly into the affected area to decrease the size and thickness of keloid scars, helping them appear smaller and flatter. Corticosteroid injections often require a series of treatments to effectively flatten the keloid, though patients may notice that their keloid feels softer after the first treatment. Typically, 50-80% of keloid scars respond to corticosteroid injections and significantly shrink after treatment.
Two newer intralesional therapies for keloid scars include bleomycin and 5-fluorouracil. Bleomycin is an anti-cancer medication typically used to destroy rapidly dividing cells, such as cancer cells. Recently, bleomycin has also been employed to treat hypertrophic and keloid scars, as it can inhibit collagen synthesis. 5-Fluorouracil is another anti-cancer drug used to treat precancers like actinic keratosis or skin cancers, including basal cell carcinomas. Fluorouracil prevents cells from making DNA and proteins, which can decrease collagen synthesis and reduce keloid scars.
VBeam laser
The Vbeam laser is regarded as the gold standard for eliminating redness. When used for keloids, the Vbeam laser specifically targets red pigmentation within the vascular component, effectively reducing discoloration and the appearance of keloids. The laser operates at a 595 nm wavelength, focusing on redness while leaving the surrounding tissue unharmed. To minimize any discomfort, the VBeam is equipped with a Dynamic Cooling Device that emits a burst of cool air before each pulse of the laser. Pulsed-dye laser therapy can address various forms of redness, including visible blood vessels, post-inflammatory hyperpigmentation, spider veins, broken capillaries, red stretch marks, and red keloid scars. Often, a series of VBeam treatment sessions spaced four to six weeks apart is necessary to achieve optimal results. There is no pain or downtime involved with the VBeam laser, allowing patients to easily receive treatment and return to their daily activities immediately after. The V-Beam is frequently combined with other therapies, such as corticosteroid injections, to reduce both the size and color of a keloid.
Surgical excision
In some cases, surgical excision may be the best option for treating keloids. Surgical removal can effectively assist patients with significant keloid scars that are large, restrict movement, or do not respond to non-surgical treatments. It is important to note that keloid surgery has a high recurrence rate due to the skin injury associated with the procedure. To reduce the chance of recurrence, some physicians may recommend pressure garments, silicone gel sheets, or corticosteroid injections after surgery to minimize the risk of the keloid reforming. Any surgical procedure carries a higher risk of side effects and infection compared to non-surgical treatments, making it essential to weigh all benefits and risks when considering surgical excision of keloids.
Cryotherapy
Cryotherapy, also known as cryosurgery, is an outdated treatment that involves applying a cooling agent, such as liquid nitrogen, directly to the keloid. This cooling agent freezes the keloid immediately upon contact, reducing the size and firmness of the scar. The keloid may blister or scab within a few days after treatment, and proper wound care will be implemented to help minimize scarring. Cryotherapy is not an effective treatment for darker-pigmented skin, as it can lead to permanent light or brown spots following the procedure. Additionally, cryotherapy is most effective for small keloids. Typically, multiple sessions are necessary to achieve optimal results. Cryotherapy may also be used following surgical excision or corticosteroid injections to help reduce the formation of scar tissue.
Radiation therapy
Radiation therapy, or radiotherapy, was once one of the most common treatments for preventing keloid formation after procedures like surgery. Radiation damages DNA, leading to cell death in keloids and the shrinking of scars. In the past, radiotherapy often resulted in side effects such as itching, peeling, and permanent color changes in the skin. Additionally, some patients reported developing cancer following keloid radiotherapy. Today, dermatologists have collaborated with oncologists to create superficial radiation therapy (SRT), which incorporates safety measures like proper dosing and shielding non-targeted body areas to ensure the safe treatment of keloids and minimize cancer risk.
Are keloid scars permanent?
Yes, without treatment, keloid scars are permanent. They extend beyond the original injury site and can develop months or even years after the initial trauma. Keloid scars arise from excess collagen produced during the wound healing process. Without treatment, they will persist on the skin for life. Fortunately, Dr. Green offers a variety of treatments for keloid scars in her private NYC dermatology office to reduce their appearance or eliminate them entirely. When you consult with Dr. Green about your keloids, she will create a personalized treatment plan to reduce the keloid for smoother skin.

Frequently Asked Questions (FAQs) about Keloids
How do you stop keloid scars from growing?
To prevent keloid scars from developing, early and consistent treatment is essential. Utilizing silicone gel sheets or silicone-based creams can help prevent keloids from forming and can also flatten and reduce scar tissue over time. It is crucial to avoid behaviors that may increase skin irritation and hinder wound healing, such as popping pimples or picking at scars, as additional trauma can lead to further keloid formation. A dermatologist can administer corticosteroid injections directly into the keloid to diminish inflammation and slow its growth. For large or persistent keloids, treatments such as laser therapy, cryotherapy, or even surgical removal followed by radiation or steroid therapy may be advised to tackle the issue and prevent recurrence. Once a keloid scar starts to grow, the best course of action is to consult with an experienced board-certified dermatologist, like Dr. Michele Green in New York City, who can develop an effective treatment plan.
How to remove keloids?
There are several options for enhancing the appearance of keloids. Patients with new keloids or scars can use silicone scar sheets to reduce their size and prevent further keloid formation. Intralesional injections are the most common treatment for keloids used by dermatologists. Corticosteroids, along with anti-cancer medications like bleomycin and 5-fluorouracil, can effectively soften and shrink keloids. The most effective method for removing keloids varies among patients, as no treatment is guaranteed to work for everyone. If you seek to remove keloids, the first step is to consult with an experienced dermatologist, such as Dr. Green in NYC, who can develop a customized treatment plan that will be effective for your keloids.
How to remove a keloid from a piercing?
Many patients wonder, “How to get rid of keloids from piercings?” or “How to remove a piercing keloid?” Body piercings are among the most common causes of keloids. The trauma caused by the piercing gun or needle triggers a wound-healing response, which can lead to an overproduction of collagen. Keloid scars often develop after piercings, particularly in individuals with darker skin tones, those who have experienced keloids before, or those with a family history of keloid scars. Although a keloid scar from a piercing can cause discomfort or itching, it typically does not hurt. Irritation is also common with keloids from piercings, as these scars are often subject to rubbing or touching. Piercings should only be performed by a reputable piercer or professional, and aftercare instructions should be diligently followed to minimize the risk of developing a keloid. Pressure garments or silicone gel sheets may be recommended if the skin around the piercing begins to thicken into a keloid. Other treatments, such as corticosteroid injections or V-Beam laser treatment, can also be considered to reduce the size and appearance of the keloid.
How to remove keloid from nose/ear/eyebrow/belly button piercing?
Any body piercing can lead to a keloid scar due to the trauma of the piercing process. Keloid scars may develop months after the initial piercing. Once a keloid begins to form, the first step is to consult a board-certified dermatologist. Smaller keloids are generally easier to treat than larger ones that have grown and hardened over a longer period. When the skin around the piercing starts to thicken, silicone gel sheets can be implemented along with pressure garments to help prevent the formation of keloids. The VBeam laser and corticosteroid injections are often used together to flatten, shrink, and reduce the red pigmentation in keloid scars from piercings on the body.
How to get rid of keloids on the ear?
Keloids on the ears can be treated similarly to those that form elsewhere on the body. They may develop on the ear and surrounding skin after an injury, such as a piercing, scratch, bug bite, tattoo, cut, or burn. Ear keloids are quite common and can grow very slowly, sometimes appearing three to twelve months after the skin injury. If the skin on the earlobe or cartilage starts to thicken around the wound, a pressure earring can be worn to help prevent a keloid from forming. For pressure earrings to be effective, they should be worn all day for six to twelve months. Other treatment options, such as intralesional injections or surgical excision, can also be utilized depending on the size and severity of the keloid scar. Following surgical excision, patients often require additional intralesional injections or cryosurgery to prevent recurrence.
How do get rid of the keloid scar on the nose?
Following a nose piercing, many individuals experience a raised nodule. This nodule may not be a keloid. However, it can be a symptom of inflammation, infection, an allergic reaction, or tissue damage. While less common, a keloid scar can form around the piercing due to excess collagen production during the healing process. A keloid on the nose manifests as a raised, tender, itchy bump that is darker than the surrounding skin. Since growth on the nose can stem from various factors, consulting an expert dermatologist, such as Dr. Green, is the best way to confirm if the growth is a keloid scar and to create a treatment plan tailored to your specific condition. A series of corticosteroid injections and V-Beam laser treatments can help reduce the redness and size of the scar, softening and potentially eliminating the keloid.
How to get rid of keloid inside nose?
Although rare, keloid scars can develop inside the nose, typically due to a nose piercing. If a keloid forms in the nose, it is essential to have it treated promptly, as it can become ulcerated (fester and cause pain) and affect the sinuses. Depending on the size and location of the scar, surgical intervention or non-surgical intralesional injections may be utilized to treat a keloid scar within the nose.
How to get rid of keloids from piercings at home?
Unfortunately, keloid scars typically cannot be treated at home. After a wound or injury to the skin, silicone gel sheets and pressure garments can be applied to the area to prevent keloid formation. However, once a keloid forms, it will not resolve without some form of intervention. Some individuals claim that onion extract, whether taken orally or applied to the skin, can help reduce the chances of keloid formation. These claims are largely anecdotal and have not been substantiated by clinical research. For safe and effective treatment of keloid scars, consult Dr. Green at her private dermatology office on the Upper East Side to discuss the best approach for your keloid scar.

How do you remove keloid scars?
While keloid scars are harmless, their presence can be frustrating and embarrassing for those affected. Keloid scars can develop anywhere on the body at the site of an injury, appearing as thick, raised, and firm growths. Unlike other hypertrophic scars, keloid scars do not resolve on their own and may extend beyond the borders of the original injury. Fortunately, treatments such as silicone gel sheets, pressure dressings, corticosteroid injections, VBeam laser therapy, cryotherapy, and surgical excision are available to help prevent and minimize the appearance of keloid scars. If you have a keloid scar from surgery, a wound, acne, or a piercing and are ready to have it treated, Dr. Michele Green in NYC is here to help.
Dr. Michele Green is an internationally renowned board-certified dermatologist with over two and a half decades of experience providing some of the world’s most discerning men and women with the best non-invasive cosmetic procedures available, including V-Beam laser and corticosteroid injections for keloid scar treatments. She is consistently identified as one of New York’s best dermatologists by Castle Connolly, New York Magazine, The New York Times, and Super Doctors for her dedication to her patients and expertise. When you consult with Dr. Green at her private dermatology office in Manhattan’s Upper East Side neighborhood, she will work with you to develop a customized keloid scar treatment plan that best suits your needs and goals. To schedule a consultation with Dr. Green, please contact us online today or call the office at 212-535-3088 to see which treatment options will work best for you.
 212-535-3088
212-535-3088