Hyperhidrosis Treatment & Excessive Sweating
Hyperhidrosis is a medical condition associated with uncontrollable excessive sweating that is unrelated to exposure to heat, exercise, or stress. This medical condition affects more than 15 million Americans, with many individuals reporting that their hyperhidrosis often interferes with their daily activities and can have a significant negative impact on their quality of life. Dr. Michele Green, in her private New York City Dermatology office, was one of the first physicians to treat patients with hyperhidrosis with Botox injections. The most commonly affected areas of the body include the armpits, palms of the hands, and the soles of the feet due to the high concentration of sweat glands in those areas. Hyperhidrosis can dictate how you live your life – keeping you inside during the summer months, limiting your clothing options for fear of sweating and staining your shirts, and preventing you from enjoying social obligations due to the potential embarrassment of lifting your arms or shaking hands. Luckily, hyperhidrosis can be diagnosed and managed with an array of non-invasive treatment options by Dr. Michele Green in NYC.
Hyperhidrosis can be caused by a variety of factors, including a genetic predisposition, an overactive thyroid, neurological conditions, or a side effect of medications. Treatment options can include prescription antiperspirants, oral medications, topical treatments, and Botox injections. Botox injections are one of the most effective and popular treatment options for reducing the symptoms of different types of hyperhidrosis. Botox works by inhibiting nerve signals that activate the sweat glands in the affected area, reducing the amount of excessive sweating experienced. Botox injection results are long-lasting, allowing patients with hyperhidrosis to experience much-needed relief and dryness. While there are few potential side effects and zero downtime associated with Botox injections, it is always critical that an experienced board-certified dermatologist, such as Dr. Green, perform Botox injections.
Dr. Michele Green in New York City is an internationally renowned board-certified dermatologist with over two and a half decades of experience providing some of the world’s most discerning individuals with the best non-invasive treatment options, including for the management of hyperhidrosis. Dr. Green takes a holistic approach, customizing each patient’s treatment plan to suit their particular concerns best. She is consistently identified as one of New York City’s best dermatologists by Castle Connolly, New York Magazine, The New York Times, and Super Doctors for her dedication to her patients and expertise. When you consult with Dr. Green regarding hyperhidrosis, she will collect a thorough medical and family history, conduct a routine physical exam, and potentially order other diagnostic tests to determine which treatment options would be best suited to your specific needs. Whether your excessive sweating is limited to your underarms or hands or involves your entire body, Dr. Green will help design the best treatment protocol for you.
What is hyperhidrosis?
Hyperhidrosis is a medical condition characterized by excessive sweating unrelated to factors that typically cause natural, healthy sweating, such as heat, exercise, or feelings of anxiety or stress. Most people with hyperhidrosis have at least one episode a week and experience excessive sweating symmetrically, with both sides of the body being affected equally. Hyperhidrosis can occur anywhere on the body where sweat glands are present but most often appears on the underarms, palms of the hands, and soles of the feet. Many report that their hyperhidrosis regularly interferes with their daily activities and negatively impacts their overall quality of life. Additionally, untreated hyperhidrosis can result in skin irritation, increased body odor, and skin infection. While there is no cure for hyperhidrosis, many topical therapies, oral medications, and office procedures exist to keep hyperhidrosis under control and help you feel like your best self again.
What are the two types of hyperhidrosis?
Primary focal hyperhidrosis
Primary focal hyperhidrosis is excess sweating caused by overactive sweat glands that are unrelated to an underlying health condition. In this type of hyperhidrosis, faulty nerve signals from the nervous system trigger the overactivity of eccrine sweat glands. Individuals with primary hyperhidrosis note that the condition usually starts to manifest in early childhood. Its cause is still debated, although researchers are beginning to show that there could be a genetic component, as it can run in families. As primary hyperhidrosis tends to affect specific areas of the body in a localized fashion, most patients with primary hyperhidrosis have a specific area of the body where excessive sweating occurs. Examples of primary hyperhidrosis include axillary hyperhidrosis (excessive sweating in the underarms or armpits), palmar (excessive sweating on the palms), and palmoplantar hyperhidrosis (excessive sweating on both the palms and the soles of the feet). There is no cure for primary hyperhidrosis. However, the symptoms can be safely and effectively managed with a variety of treatment options provided by a board-certified dermatologist like Dr. Green. Dr. Green may recommend oral or topical medications, prescription antiperspirants, Botox injections, or a unique combination of treatment options.
Secondary hyperhidrosis
Secondary hyperhidrosis is excessive sweating caused or triggered by an underlying condition or side effect of a medication or supplement. Medical conditions that might induce secondary hyperhidrosis include infectious diseases (malaria, tuberculosis, HIV), neurologic conditions (anxiety, stress, panic attacks), menopause, diabetes, obesity, low blood sugar, Parkinson’s disease, hyperthyroidism, and leukemia. Secondary hyperhidrosis usually involves generalized excessive sweating that affects the entire body rather than a specific area. In some cases, secondary hyperhidrosis can sometimes be cured by ceasing the medication/supplement or addressing the underlying condition causing it. Regardless, secondary hyperhidrosis can effectively be managed with various treatment options provided by a board-certified dermatologist like Dr. Green in NYC.
What are the symptoms of hyperhidrosis?
The main symptom of hyperhidrosis, and what separates it from normal sweating, is excessive sweating that is unrelated to exercise, stress, or exposure to heat. Individuals who have hyperhidrosis may experience excessive sweating without any exertion and may develop symptoms such as body odor, skin irritation (itching or inflammation), and frequent skin infections. Patients with primary hyperhidrosis will most commonly be affected in certain body areas, including the hands, feet, face, and underarms. Patients with secondary hyperhidrosis typically experience generalized excessive sweating that is not specific to any specific area of the body but rather affects the entire body. Unfortunately, due to the nature of this medical condition, many patients also experience that their hyperhidrosis disrupts their normal daily activities, causes low self-esteem and self-consciousness, or has another negative impact on their overall quality of life. An experienced board-certified dermatologist, such as Dr. Michele Green in NYC, can diagnose your hyperhidrosis and recommend a customized combination of treatment options to help manage symptoms and improve your quality of life.
What causes hyperhidrosis?
The root cause of hyperhidrosis is an overactivity of eccrine sweat glands in the body. The eccrine sweat glands account for 2 to 4 million of the sweat glands in the body, with the highest concentration of sweat glands found in areas of the body such as the feet, hands, and underarms. When body temperature rises, the sympathetic nervous system releases acetylcholine, signaling the eccrine sweat glands to secrete water and minerals to lower body temperature. Once body temperature is regulated, the signaling is “turned off.” However, for individuals with hyperhidrosis, this signaling is never turned off, resulting in abnormal and excessive sweating. While some individuals develop hyperhidrosis due to genetic predisposition or faulty nerve signals from the nervous system, excessive sweating can sometimes be a sign of an underlying medical condition or even a side effect of certain medications or supplements. When excessive sweating occurs for an unknown reason, suddenly interferes with your usual daily activities, negatively impacts your quality of life, or causes other symptoms, it is important to meet with an experienced healthcare provider, like board-certified dermatologist Dr. Michele Green in NYC, to better understand the possible causes.

What is axillary hyperhidrosis?
Axillary hyperhidrosis is excessive sweating that affects the underarms or armpits. Axillary hyperhidrosis can be either primary or secondary hyperhidrosis, but most cases are primary. While it is normal for people to sweat from their underarms to regulate the body’s temperature as a response to exercise, heat, or stress, excessive sweating due to hyperhidrosis can occur at any time and can be disruptive to one’s daily activities, causing social anxiety, embarrassment, and a worse overall quality of life. This kind of excessive sweating can occur due to hormonal imbalances, menopause, hyperthyroidism, or a genetic predisposition to overactive sweat glands, in addition to being a potential side effect of some medications and supplements. Like other types of hyperhidrosis, axillary hyperhidrosis can be managed with a variety of treatment options available at Dr. Green’s private dermatology office in Manhattan’s Upper East Side neighborhood. Popular treatment options include Botox injections, topical and oral medications, and prescription antiperspirants.
What is palmar hyperhidrosis?
Palmar hyperhidrosis is classified as excessive sweating of the palms of the hands. Similar to axillary hyperhidrosis, abnormal sweating of the hands is typically associated with primary hyperhidrosis. Palmar hyperhidrosis can be difficult to cope with, especially in professional settings, where shaking hands is often necessary. This issue has social ramifications, and it can be very embarrassing for patients suffering from chronic excessively sweaty hands. It is best to consult with a board-certified dermatologist like Dr. Green to learn how to treat sweaty palms with oral medications and in-office treatments. Botox injections are an extremely safe and effective treatment option for addressing palmar hyperhidrosis if antiperspirants do not work to decrease sweating. Botox treatment can keep palms dry for up to 4 months and can be repeated for decreased sweating.
What is plantar hyperhidrosis?
Plantar hyperhidrosis is a type of primary hyperhidrosis that affects the soles of the feet. Plantar hyperhidrosis affects many individuals and can often cause fungal infections of the feet. The initial symptoms of plantar hyperhidrosis are a slight foot odor, a white-hued residue on your feet, or damp socks or stockings. This condition can be very embarrassing for individuals who suffer from it. Botox injections are a very effective treatment option for managing the symptoms of plantar hyperhidrosis, and several injections across the foot surface can safely and effectively be used to alleviate this problem. However, Dr. Green does not treat plantar (foot) based hyperhidrosis. It is important to always seek hyperhidrosis treatment, especially Botox injections, from an experienced healthcare provider, such as a board-certified dermatologist. Working with a dermatologist for the treatment of hyperhidrosis will help guarantee that your plan is safe and effective and provides you with the best results.
What is gustatory hyperhidrosis?
Gustatory hyperhidrosis, also commonly referred to as Frey’s syndrome, is excessive sweating while eating. This type of hyperhidrosis typically presents on the forehead, neck, scalp, and upper lip. It can result from damage to the parotid gland and is typically a side effect of surgery, among other medical causes. There is no cure for this type of hyperhidrosis. Still, symptoms can be safely and effectively managed with many of the same treatment options used to treat other types of hyperhidrosis, including Botox, topical antiperspirants, and topical anticholinergics.
How do you cure hyperhidrosis?
Currently, there is no cure for primary hyperhidrosis. Primary hyperhidrosis is uncontrollable excessive sweating that is not caused by an underlying medical condition or a side effect of medications/supplements. Secondary hyperhidrosis, which is caused by an underlying medical condition or a side effect of medication, can potentially be cured if the underlying condition is resolved or the medication causing excessive sweating ceases. In either case, patients can safely and effectively manage the symptoms of their hyperhidrosis with various treatment options through a dermatologist like Dr. Michele Green in NYC. When you consult with Dr. Green at her private dermatology office in Manahattan’s Upper East Side neighborhood, she will determine the best treatment options for your specific case depending on your medical and family history, the type of hyperhidrosis you have, the area of the body affected, and the specific concerns you have to stop you from sweating uncontrollably and excessively and improve your overall quality of life.
How to treat hyperhidrosis with in-office procedures
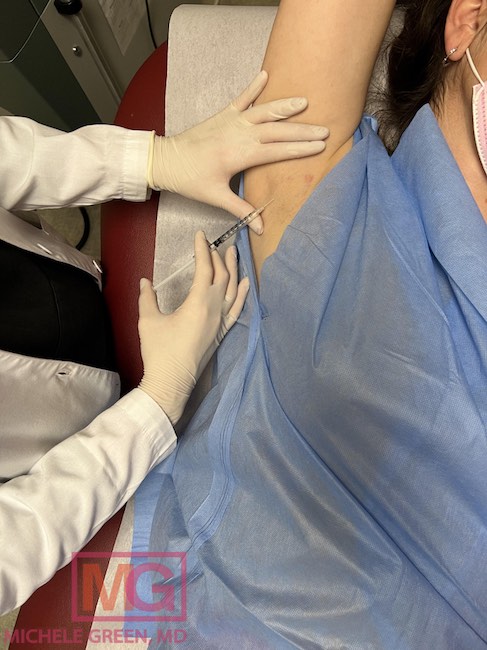
Botox injections for the treatment of hyperhidrosis
Botox, a neurotoxin composed of botulinum toxin, has been approved by the FDA for the medical treatment of axillary hyperhidrosis or excessive sweating in the underarms. Botox is often used off-label by experienced dermatologists to treat palmar hyperhidrosis. Botox acts by inhibiting nerve signaling to sweat glands to reduce sweat secretion. There is no downtime or recovery time associated with treatment, and patients can return to their regular daily activities immediately following the procedure. The most common side effects of Botox injections include a mild amount of swelling, bruising, and tenderness at or near injection sites, which resolve on their own within two weeks of treatment. It takes up to two weeks for the effects of Botox injections to kick in, after which they can last from 4 to 6 months, depending on the area being treated. Patients are advised to come in for regular treatment sessions to maintain optimal results. Botox injections are Dr. Green’s preferred treatment option for hyperhidrosis due to their safety and efficacy in providing relief from excessive sweating.
Brella by Candesant Biomedical
Brella by Candesant Biomedical is a new innovative, non-invasive treatment option for axillary hyperhidrosis that was FDA-cleared in April 2023. Brella is the first and only patented medical device that utilizes targeted alkali thermolysis (TAT) technology to affect the sweat glands, effectively reducing excessive sweating in the underarms. When the Brella sodium patch is applied to the underarms, the heat energy generated when sodium and sweat come into contact has a localized effect on the sweat glands to reduce underarm sweating. This unique hyperhidrosis treatment entails a healthcare provider’s professional application of the patch to the armpit, which is removed after approximately three minutes. The treatment is entirely non-invasive and pain-free, meaning patients can easily resume most of their usual daily activities following the procedure. Each Brella sodium patch is single-use and disposable, with results from each treatment session lasting 3-4 months.
Iontophoresis for palmoplantar hyperhidrosis
Iontophoresis is an FDA-approved procedure for treating palmar and plantar hyperhidrosis. It involves sitting with your hands and feet submerged in a shallow tray of tap water. As you sit, a machine delivers low electrical currents that travel through the water. Experts believe that electric currents block the sweat glands and prevent sweating. This treatment needs to be repeated several times a week to be effective, followed by regular treatment sessions to maintain sweat relief.
miraDry microwave thermolysis for axillary hyperhidrosis
miraDry® is an FDA-approved treatment for axillary hyperhidrosis. It utilizes a handheld device that delivers precise microwave energy to the affected areas of the underarms, destroying the sweat glands. Once the sweat glands are destroyed, they do not regenerate, eliminating excessive sweating. Clinical studies have suggested that miraDry can reduce excessive sweating in the axillae by up to 82% after two treatment sessions.
Surgical treatment for hyperhidrosis
Many patients ask, “What is hyperhidrosis surgery?” Two different surgical procedures can be performed for hyperhidrosis: endoscopic thoracic sympathectomy (ETS) and sweat gland removal. ETS involves a surgeon making very small incisions in the skin to clamp off or burn the sympathetic nerve endings, inhibiting the signals that cause sweating. Sweat gland removal is a last-resort treatment for very severe cases of hyperhidrosis when all other therapies have failed. This minimally invasive surgical treatment entails the complete removal of sweat glands using lasers, liposuction, or curettage techniques. Surgical procedures are intended for patients with primary hyperhidrosis who experience localized excessive sweating on the palms of the hands, soles of the feet, or under the arms.
The effects of these procedures are permanent and irreversible. As with any surgical procedure, there is some risk of infection. Patients may develop compensatory sweating, in which other areas of the body sweat more than usual to compensate for the areas affected by the procedure. Other potential side effects include nerve damage, irregular heartbeat, and low blood pressure. Many patients prefer to have Botox injections for hyperhidrosis treatment, as there is little risk and no downtime involved with the procedure.
Oral medications for hyperhidrosis treatment
Anticholinergic medications
Anticholinergics are oral medications that chemically block nerve endings of eccrine sweat glands to inhibit nerve signaling and prevent excessive sweating. The most commonly prescribed Anticholinergics include glycopyrrolate, oxybutynin, benztropine, and propantheline. Not all of these medications are FDA-approved for this condition, and many of them are used in an “off-label” capacity. Anticholinergics are typically prescribed for patients with secondary hyperhidrosis who experience generalized excessive sweating, as the medications work systemically. While these medications work well and effectively treat hyperhidrosis, they are not without side effects, causing dry mouth and blurred vision, among other medical issues.
Antidepressants
Benzodiazepines are a group of antidepressants that have also been found useful in treating hyperhidrosis. They work by controlling anxiety, which often results in excessive sweating. These systemic medications work by controlling the central nervous system — by doing so, they mitigate the physical aspects of sweating, often seen during episodes of anxiety.
Beta Blockers
Beta-blockers have also been successful in treating excessive sweating. Their mechanism of action is similar to that of antidepressants in that their effects work on the central nervous system. The most common beta blocker used for hyperhidrosis is propranolol, which is also commonly prescribed for anxiety disorders. Sweating is a common physical manifestation of anxiety for individuals who suffer from it, which is why these drugs work well for excessive sweating.

Topical prescriptions to treat hyperhidrosis
Aluminum chloride
The most common ingredients in prescription deodorants for hyperhidrosis include aluminum chloride and aluminum chloride hexahydrate. When aluminum chloride mixes with sweat, a precipitate is created that forms a plug in the sweat gland ducts and prevents sweat from being secreted. Drysol is a common topical antiperspirant that is available as a prescription containing 20 percent aluminum chloride. It is not recommended that Aluminum chloride be used as a long-term solution as it can cause skin and eye irritation in some individuals. If you experience skin irritation from using aluminum chloride, you should discontinue use and consult Dr. Green. In most instances, a prescription for topical hydrocortisone usually clears up the skin irritation in a few days. During the 1960s, many people speculated that aluminum was the cause of Alzheimer’s disease; however, this was disproven through various modern scientific studies. Furthermore, according to the National Cancer Institute, there is no evidence that deodorants and antiperspirants cause breast cancer, even though it is often applied on the underarms near the breasts.
Glycopyrronium tosylate
Glycopyrronium tosylate is a topical anticholinergic treatment that is FDA-approved under the brand name Qbrexza. Qbrexza can be used to manage hyperhidrosis in children as young as nine years old. The cloths come in a pre-moistened, individually wrapped, single-use package, making them readily available for use. Qbrexza is convenient due to its packaging, which makes it easy for teens and adults to carry and use while exercising to minimize excessive sweating. The pre-moistened clothes can be used to treat the underarms and groin area.
Over-the-counter topicals to manage hyperhidrosis
Many new products on the market are being formulated and researched to treat hyperhidrosis, including antiperspirant deodorants, hand creams, foot creams, and body antiperspirants. Deodorants were initially created to combat body odor. Antiperspirants, on the other hand, work to decrease sweat production in the applied areas. Deodorants should also contain antiperspirant properties to work effectively against controlling sweat. Active ingredients to look for in antiperspirants include aluminum chloride, aluminum chlorohydrate, and aluminum zirconium. These ingredients hinder sweat production by combining with moisture (sweat) to form a gel that sits on top of the skin. This gel obstructs the distal sweat gland ducts and forms a temporary plug that blocks sweat from flowing out of the skin. Antiperspirant deodorants can come in different forms, like sticks, gel, sprays, and wipes.
How to treat hyperhidrosis naturally
Hyperhidrosis is a chronic condition that can result from genetic predisposition or as a side effect of certain medical conditions, medications, or supplements. Many patients wonder if there are any natural remedies that they can try before turning to medications or procedures. Sage tea is often recommended due to its astringent properties that can minimize sweating, and chamomile tea can increase relaxation to reduce stress and sweating. Acupuncture can also provide some benefits for patients with hyperhidrosis, as treatment may help to regulate the nervous system. There is little research, however, looking into how effective natural remedies are in treating hyperhidrosis. For many, a combination approach of treatments is often best for reducing excessive sweating. If you are interested in natural remedies for hyperhidrosis treatment, consult with a board-certified dermatologist like Dr. Green to ensure that the treatments are both safe and effective.

FAQs about hyperhidrosis
How common is hyperhidrosis?
Hyperhidrosis is a medical condition affecting nearly 3 percent of people in the United States, equivalent to about 15 million Americans. While individuals who suffer from excessive sweating may feel alone and embarrassed, there has been an increase in media coverage of the condition, which has helped to normalize it. Prominent figures such as Chrissy Teigen have taken to social media to discuss their experience with hyperhidrosis, increasing the visibility of the condition and helping others feel more comfortable seeking treatment. Chrissy Teigen even revealed how she used Botox to eliminate her severe underarm sweating. De-stigmatizing and normalizing treatments for hyperhidrosis is incredibly important, as treatments like Botox can have a significant positive impact on one’s overall quality of life and restore feelings of self-confidence.
What does it mean when you sweat easily?
Some individuals are predisposed to sweat in the presence of any rise in body temperature, no matter how small. These individuals likely sweat easily due to a heightened nervous system response to stress, heat, or exercise. Individuals with a larger body size may also sweat easily as more body mass can generate more heat. However, being able to sweat easily does not mean that you have hyperhidrosis. Sweating is a normal and healthy function of the human body, helping to keep it cool. Hyperhidrosis is a medical condition characterized by uncontrollable excessive sweating that is not in response to a rise in body temperature from stress, heat, or exercise. Hyperhidrosis can appear in local areas, such as the armpits, palms, or soles of feet, or generally across the body.
What does excessive sweating mean?
Many patients wonder, “What does excessive perspiration mean?” Excessive sweating in the absence of a rise in body temperature is known as hyperhidrosis. For individuals with primary hyperhidrosis, there is no direct cause of excessive sweating. These patients often have a genetic predisposition toward hyperhidrosis, with many members of their family also having it. Individuals with secondary hyperhidrosis experience excessive perspiration as a result of hormone fluctuations, underlying medical conditions, or a side effect of certain oral medications and supplements.
Why do I have hyperhidrosis?
Some patients experience hyperhidrosis due to a genetic predisposition for uncontrollable excessive sweating, also known as primary hyperhidrosis. Patients with hyperhidrosis often experience excessive sweating in childhood, typically occurring in localized areas such as the underarms, palms of the hands, or soles of the feet. Some patients experience hyperhidrosis as a result of an underlying health condition (diabetes, Parkinson’s disease, thyroid disorders, certain cancers), changes in hormone levels (menopause, pregnancy), or medications (certain antipsychotics and opioids).
Is hyperhidrosis dangerous?
In general, hyperhidrosis is harmless and not medically dangerous, nor is it usually indicative of a more serious underlying medical condition. Individuals experiencing hyperhidrosis can typically engage in regular daily activities successfully. Still, for many, excessive sweating will most likely disrupt daily activities or negatively impact their overall quality of life. Additionally, primary hyperhidrosis can also increase the risk of skin infections, as excessive sweat breaks down the skin (maceration), allowing bacteria and viruses to enter the skin more easily. While excessive sweating is characteristic of hyperhidrosis, it can sometimes be a sign of a more serious medical condition if it occurs suddenly, only presents as intense night sweats, or is accompanied by other unrelated symptoms. Seek immediate medical attention if the hyperhidrosis is accompanied by chest pain, lightheadedness, or nausea.
How do I know if I have hyperhidrosis
Hyperhidrosis is a medical condition that involves uncontrollable excessive sweating from any part of your body unrelated to exercising or being exposed to hot temperatures. Excessive sweating associated with hyperhidrosis usually occurs symmetrically, affecting both sides of the body equally. In some cases, patients may experience sleep hyperhidrosis or night sweats. If you only experience night sweats, be sure to consult an experienced medical professional, as this can sometimes be indicative of a larger systemic issue. Otherwise, you don’t need a “Do I Have Hyperhidrosis Quiz” to confirm that you are living with hyperhidrosis. If you are experiencing moderate to severe excessive sweating on your hands, feet, underarms, face, or across other parts of your body that are unrelated to normal, healthy sweating, you likely have hyperhidrosis. Fortunately, there are many non-invasive treatment options available at Dr. Green’s private dermatology office that can be used to help manage symptoms and reduce excessive sweating.
Does hyperhidrosis go away?
Patients with hyperhidrosis often ask, “Can hyperhidrosis go away?” Secondary hyperhidrosis can go away. This type of hyperhidrosis is caused by an underlying medical condition or a side effect of a medication or supplement. With secondary hyperhidrosis, treating the underlying condition or changing medications or supplements can vastly reduce or get rid of hyperhidrosis. On the other hand, there is no direct cause for primary hyperhidrosis, though there may be a genetic component to its development. There is no cure for primary hyperhidrosis, and it will not go away on its own. Luckily, there are many different treatment options, including Botox injections, topical therapies, and oral medications that effectively treat and manage hyperhidrosis. If you are ready to curb excessive sweating for good, consult with Dr. Green today to find out the best course of action for your specific type of hyperhidrosis.
Can you develop hyperhidrosis?
Yes, it is possible to develop hyperhidrosis. Secondary hyperhidrosis can appear as a result of certain medical conditions, hormonal fluctuations, medications, and supplements. Common medical conditions that cause hyperhidrosis to develop include diabetes, hyperthyroidism, and Parkinson’s disease. Women undergoing menopause or pregnancy can develop excessive sweating as a result of fluctuations in estrogen and progesterone. Antipsychotic medications, such as haloperidol, clozapine, and citalopram, can cause hyperhidrosis to develop, likely through increased acetylcholine activity. When taken in high doses, iron and zinc supplements can also cause excessive sweating. If you have developed hyperhidrosis, it is essential to consult with a healthcare provider or a board-certified dermatologist like Dr. Green to determine the root cause of your hyperhidrosis and obtain proper treatment.
How do I get my armpits to stop sweating?
Axillary hyperhidrosis, or excessive sweating of the armpits, is one of the most common forms of hyperhidrosis. There are many different ways to treat and manage underarm sweating, including Botox injections. Botox works to inhibit nerve signaling in an injected area — when injected into the underarms, Botox decreases signaling to the eccrine sweat glands, resulting in decreased sweat production. Botox injections are incredibly safe and effective for axillary hyperhidrosis, especially in the hands of an expert board-certified dermatologist like Dr. Green. After each treatment session, patients look forward to managing symptoms for four to six months before another session is needed. Other options for managing excessive armpit sweating include topical antiperspirants, Qbrexza anticholinergic wipes, and oral medications. When you consult with Dr. Green, she will assess your medical history and concerns to devise the best treatment plan to leave you with sweat-free underarms.

How to cure sweaty hands and feet permanently
While there is no way to cure hyperhidrosis in the hands and feet permanently, many treatment options are available to provide long-lasting relief. Similar to axillary hyperhidrosis, Botox injections can also be used off-label to treat palmar hyperhidrosis. By injecting Botox into the palms, patients can look forward to decreased sweat production for four to six months. Some providers may also use Botox off-label to treat plantar hyperhidrosis.
Iontophoresis is a popular treatment for palmoplantar hyperhidrosis, or excessive sweating in the palms and soles of the feet. It involves submerging the hands and feet in a shallow tub of water. Electrical currents are then delivered into the water to disrupt nerve signaling to the eccrine sweat glands and reduce sweat secretion. Typically, an initial series of treatments is required, followed by maintenance sessions to provide continued sweat relief.
Does insurance cover Botox for hyperhidrosis?
Botox is an FDA-approved treatment option for managing symptoms of axillary hyperhidrosis, and some private health insurance companies will cover it. Typically, insurance companies will only cover Botox injections for axillary hyperhidrosis (excessive underarm sweating) after other prescribed antiperspirants, topical treatments, and oral medications have been tried. It is important to consult with your specific health insurance provider directly to determine if your plan covers Botox injections for hyperhidrosis.
Who treats hyperhidrosis?
Hyperhidrosis is a medical condition that can be diagnosed and treated by a certified healthcare professional, such as a board-certified dermatologist. Dr. Michele Green is a board-certified dermatologist in the Upper East Side of Manhattan with over 25 years of experience providing some of the world’s most discerning individuals from around the world with the best non-invasive cosmetic and medical dermatological procedures. Among the treatment options offered at her private dermatology office, Dr. Green provides what has been described as the best Botox injections in NYC, including for hyperhidrosis. In addition to Botox, a dermatologist like Dr. Green may recommend prescription antiperspirant deodorants, supplements, or medications to manage the symptoms of hyperhidrosis. Primary care physicians, internists, surgeons, and neurologists are different types of doctors who may also be able to assist with managing the symptoms of hyperhidrosis. To diagnose hyperhidrosis, your healthcare provider may perform a physical exam, collect medical and family history, and potentially request diagnostic tests such as a urine, blood, or starch-iodine test to measure excessive sweating.
How do I get started with treatment for my hyperhidrosis today?
Hyperhidrosis is a medical condition characterized by uncontrollable excessive sweating independent of any factors like exercise, stress, or heat. Hyperhidrosis can regularly interfere with one’s daily activities and significantly negatively impact one’s overall quality of life. For many, it is not just frustrating but embarrassing and causes anxiety regarding their choice of attire and social interactions. Depending on the underlying causes of hyperhidrosis, there may or may not be a cure. However, regardless of the cause of your hyperhidrosis, symptoms can be managed with a variety of safe and effective treatment options provided by a board-certified dermatologist like Dr. Michele Green in New York City. Common treatment options for hyperhidrosis include topical and oral medications, prescription antiperspirants, and Botox injections. If excessive sweating interferes with daily activities, causes frequent skin infections, affects self-confidence, or otherwise causes discomfort, Dr. Green in NYC is here to help.
Dr. Michele Green is an internationally renowned board-certified cosmetic dermatologist with over two and a half decades of experience providing her patients worldwide with the best non-invasive treatment options available, including Botox injections for hyperhidrosis. Offering the most cutting-edge treatments and utilizing innovative techniques, Dr. Green is consistently identified as one of the best physicians in New York City by Castle Connolly, New York Magazine, Super Doctors, and The New York Times. When you consult with Dr. Green at her private dermatology office in the Upper East Side neighborhood of Manhattan, she will work with you to develop a customized treatment plan that is best suited to your unique skin concerns and goals. To schedule a consultation with Dr. Green and learn more about how to deal with hyperhidrosis and treat excessive sweating with Botox injections, call the NYC office at 212-535-3088 or contact us online today.
 212-535-3088
212-535-3088 