Cystic Acne Treatment
Cystic acne is a serious, inflammatory type of acne that forms deep within the skin. Its appearance can be upsetting and painful, often causing people to feel self-conscious about their looks. Luckily, many over-the-counter topical treatments, skincare products, oral medications, and in-office procedures are available to help eliminate cystic acne breakouts at Dr. Michele Green’s private New York dermatology office. It’s important to treat cystic acne quickly, as scars that develop can be more challenging to treat than the initial breakouts. At her private, boutique dermatology office in NYC, Dr. Green will help you clear your cystic acne and achieve a clear, healthy, and radiant complexion.
There are many treatment options and preventive strategies available to manage cystic acne and prevent future breakouts. Dr. Green’s exclusive skincare line, MGSKINLABs, offers products featuring acne-fighting ingredients such as benzoyl peroxide, salicylic acid, and retinol to reduce oil and combat acne. Since cystic acne occurs deep within the skin, oral medications such as antibiotics, Spironolactone, or Accutane may be recommended. Dr. Green also treats cystic acne with corticosteroid injections, acne surgery, HydraFacials, and chemical peels. Often, the most effective approach combines topical treatments, oral medications, and in-office procedures. Dr. Michele Green in NYC is an expert in acne and scar treatment, creating a personalized plan tailored to your skin type, tone, and type of acne breakouts.
Dr. Michele Green is a globally recognized, board-certified dermatologist with over 25 years of experience in creating personalized acne treatment plans tailored to each patient’s skin condition, type, tone, and specific acne types. She is consistently named one of New York’s top healthcare providers by Castle Connolly, New York Magazine, The New York Times, and Super Doctors, thanks to her dedication and expertise. Dr. Green emphasizes building strong relationships with her patients, taking time to understand their skin issues and customizing treatment plans to meet their individual needs and goals. When you consult with her, she will recommend a personalized combination of topical and oral medications, specially formulated skincare products, and in-office procedures to effectively address your skin concerns and help you achieve clear, radiant skin.
What is Cystic Acne?
A cyst is a type of acne lesion characterized by a large, red, painful bump that doesn’t develop a “head.” Cystic acne usually contains pus and forms deep beneath the skin’s surface, making most over-the-counter treatments ineffective. It is a more severe, highly inflammatory type of acne with a greater risk of scarring. Common treatments include oral antibiotics, Accutane (Isotretinoin), and Spironolactone. While topical treatments can assist oral medications in managing cystic acne, they generally cannot effectively clear cystic breakouts on their own because they don’t penetrate deeply enough to treat and prevent these lesions. Still, it remains important for patients with acne-prone skin to use skincare products suited to their specific skin type. Consulting with an experienced, board-certified dermatologist like Dr. Michele Green provides the best approach for treating and preventing breakouts and acne scars.

Accutane 6 months – before and after
What is the main cause of cystic acne?
Cystic acne lesions develop when excess oil, bacteria, and dead skin cells clog the sebaceous glands at the base of hair follicles in the skin. Cystic acne breakouts most often affect the face but can appear anywhere oil glands exist, such as the back, chest, buttocks, shoulders, and neck. Genetics can influence cystic acne development, as the chances of experiencing these breakouts tend to be higher if one or both parents have a history of them. Some people are more susceptible to cystic acne because of their skin’s natural oil production. Hormonal changes during puberty, pregnancy, menstruation, and menopause can increase the risk of cystic acne. While anyone can develop cystic acne, it primarily affects teenagers, those with a genetic predisposition, and adults with hormonal imbalances. Because inflammation from cystic acne can occur very deeply, over-the-counter products may be ineffective, making professional treatment by a board-certified dermatologist, such as Dr. Green, essential to prevent scarring and long-term skin damage. During your consultation, Dr. Green will review your complete medical and family history, examine your skin, and order specific lab tests to identify the root causes of your acne and determine the best treatment plan. Regardless of the cause of your cystic acne, Dr. Green is committed to helping you treat it and achieve a clear, smooth, and beautiful complexion that lasts.
Will cystic acne go away on its own?
Cystic acne is unlikely to clear up without treatment. Unlike other types of acne, cystic acne occurs when bacteria become trapped, resulting in inflammation that extends deep beneath the skin’s surface. Without intervention, cysts can take weeks to months to resolve on their own, and the painful, pus-filled lesions may rupture beneath the skin, permanently damaging nearby tissue and leading to acne scars. Additionally, cystic acne causes lasting damage to the surrounding skin, making scars more difficult to treat than the acne lesions themselves. To prevent skin damage and avoid permanent scarring, it is essential to seek treatment from a board-certified dermatologist, such as Dr. Green, as soon as cysts appear.
Dermatology Acne Treatments for Cystic Acne in the Office
Acne surgery: How to shrink cystic pimples
The quickest way to reduce a painful cyst is with an in-office treatment performed by a board-certified dermatologist, such as Dr. Michele Green in New York. Acne surgery is an in-office procedure that involves creating an opening in active acne lesions, removing the contents with a comedonal acne extractor, and administering corticosteroid injections directly into the emptied lesions. The steroid injections can help decrease some of the inflammation commonly linked to cystic acne, which may lower the risk of developing scars. This quick treatment removes sebum and dead skin cells trapped in clogged pores, the main causes of acne. Extracting the contents of active lesions prevents scar formation and facilitates the skin’s healing process. While acne surgery is effective for active blemishes, it does not prevent new lesions from forming. Patients with cystic acne who undergo this procedure usually still need to take oral medications and use topical treatments to resolve their breakouts completely. For long-term control, Dr. Michele Green in NYC may combine these procedures with oral medications, personalized skincare routines, and laser treatments to help prevent future breakouts.

VBeam- 4 sessions
VBeam Laser for acne blemishes
The VBeam laser is regarded as the top choice for eliminating facial redness, including that caused by acne. It operates at a wavelength that specifically targets red pigment, leaving the surrounding skin unharmed. This laser treatment also kills acne-causing bacteria, reduces inflammation, and stimulates the production of new collagen, leading to fewer breakouts and improved skin texture. There is no downtime, allowing patients to resume their daily activities immediately after the procedure and easily schedule follow-up sessions. The treatment is painless, and the laser features a dynamic cooling device that blows cool air before each laser pulse to enhance patient comfort. Most patients require 4 to 6 VBeam sessions to eliminate redness fully.
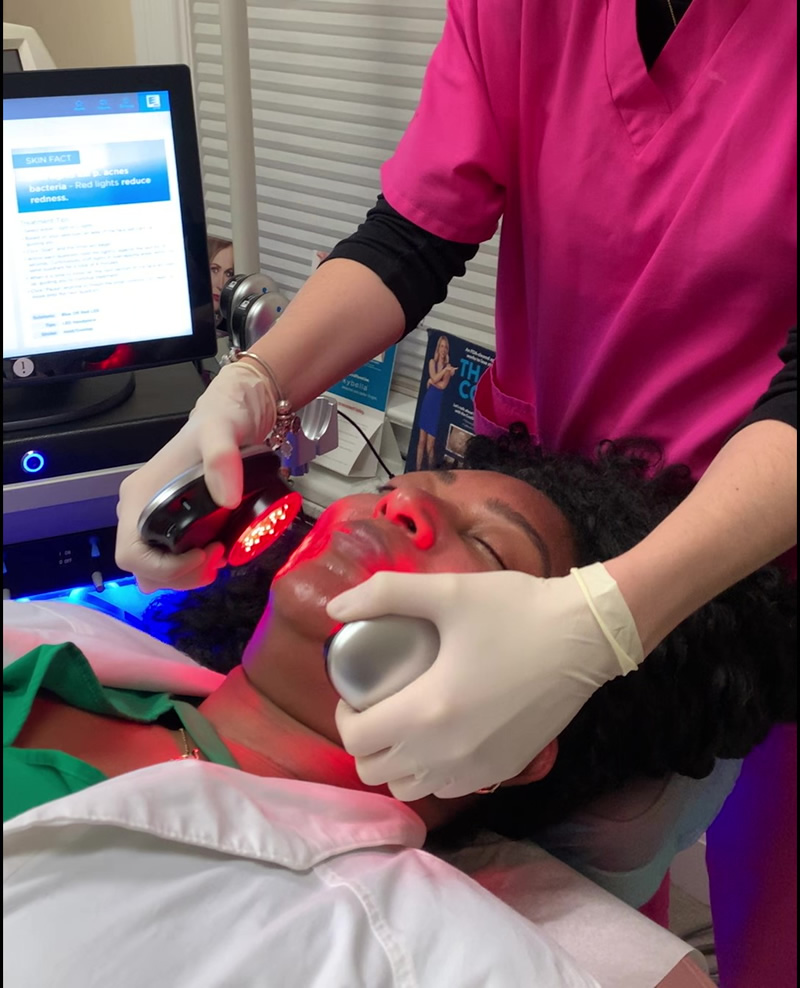
HydraFacials to treat acne breakouts
A HydraFacial is a three-step, medical-grade facial that emphasizes deep cleansing, gentle exfoliation, and intense skin nourishment. This treatment uses a handheld device to deliver a mix of serums through a patented vortex fusion tip. The first step involves cleansing the skin by suctioning away dirt, debris, and dead skin cells. The second step applies a chemical peel that combines salicylic and glycolic acids to boost skin cell turnover, break down excess oil that clogs pores and causes acne, and further exfoliate the skin. The third step infuses the skin with powerful antioxidants to nourish and reinforce its natural protective barrier, helping to prevent toxins and environmental irritants from penetrating.
HydraFacial treatments can also be enhanced with LED light therapy and targeted boosters. Red LED light reduces inflammation and redness, while blue LED light eliminates acne-causing bacteria on the skin’s surface. HydraFacial boosters are designed to address various skin concerns, including acne, dryness, redness, and pigmentation. The Murad Clarifying Booster is an excellent addition to an acne-focused HydraFacial. This booster contains salicylic acid for a deeper cleanse and green tea extract to help soothe irritated skin. When you schedule a HydraFacial with Dr. Green’s office, she will collaborate with you to customize your treatment, ensuring it targets your primary skin concerns and leaves you with a healthy, radiant complexion.
Chemical Peels to treat acne
A chemical peel is a non-invasive skin resurfacing treatment designed to speed up skin cell turnover, helping to slough off dead skin cells, debris, and dirt more quickly than they would naturally. This treatment can remove dead skin cells and sebum from clogged pores, revealing a healthier complexion with more even tone and texture, while also helping to prevent or clear up blemishes. The chemical solution causes the peeling of dead skin cells, exposing new, unblemished skin that replaces older, damaged, and dead cells. Different types and strengths of chemical peels are available to target various skin concerns, including hyperpigmentation, acne scars, fine lines, rosacea, and sun damage, among others. During your consultation, Dr. Green can determine the appropriate type and strength of chemical peel to effectively treat your skin condition and prevent breakouts and acne scars.

Accutane 6 months – before and after
Cystic Acne Treatment: Oral Medications
Oral antibiotics like Doxycycline and Tetracycline effectively treat mild to severe inflammatory acne, including cystic acne. These antibiotics help reduce and eliminate acne-causing bacteria on the skin’s surface. The frequency and strength of your prescription may vary depending on the severity of your skin condition. While taking oral antibiotics, it is generally recommended to supplement with probiotics to support gut health.
Spironolactone (Aldactone) is a medication prescribed to women to regulate androgen hormones that contribute to acne breakouts. Increased androgen levels can lead to an overproduction of sebum in the skin, causing cystic acne lesions. Individuals prone to acne, those experiencing hormonal-related acne, and especially women with Polycystic Ovary Syndrome often find significant relief from their breakouts by taking spironolactone.
Oral contraceptives, also known as birth control pills, can help regulate the hormones that surge during a woman’s menstrual cycle and reduce acne flare-ups associated with those hormonal changes. Birth control pills prevent hormonal acne by maintaining hormonal balance. Effective oral contraceptives for acne should contain hormones like estrogen and progestin. Yaz, Ortho Tri-Cyclen, and Estrostep are three FDA-approved oral contraceptives specifically formulated to treat women with hormonal acne. Possible side effects of birth control pills may include weight gain, nausea, mood swings, and a higher risk of blood clots. Women should avoid smoking while taking oral contraceptives, as it significantly increases the risk of developing blood clots.
Oral isotretinoin is one of the most effective treatments for cystic acne. In the past, Accutane (the brand name for isotretinoin) was reserved only for the most severe cases of recalcitrant nodular or cystic acne. However, Accutane is now used to treat both moderate and chronic acne breakouts, especially those that have not responded to other treatments. Typically, a course of Accutane lasts around 20 weeks. However, the duration may vary depending on the patient’s response—ninety-five percent of patients treated with Accutane experience a permanent reduction in their acne. The remaining 5% usually achieve full clearance after a second course of treatment.
The most common side effects of Accutane include dryness of the lips, skin, and eyes. Since Accutane is processed in the liver, it is important to avoid alcohol and limit dietary fats during treatment. Strict sun protection and the use of sunscreen are necessary because Accutane is photosensitizing and can increase your risk of sunburn while treating acne. The FDA regulates Accutane prescriptions, and patients must have monthly visits and blood tests to get a prescription from a board-certified dermatologist. Additionally, Accutane can cause serious congenital disabilities if taken during pregnancy—patients who can become pregnant must have monthly pregnancy tests and either pledge to abstain from sex or use two forms of birth control during treatment.
What is the best treatment for cystic acne?
There isn’t a single “best” treatment for cystic acne because many factors, including hormone levels, genetics, lifestyle, and skin sensitivity, can influence the condition. What works well for one person might not work for another, so treatment is often personalized. Some patients respond best to oral medications, such as isotretinoin, while others benefit more from topical retinoids, in-office procedures, or a combination of these approaches. The most effective plan typically involves tailoring treatment to the severity of acne, the patient’s skin type, and their long-term goals for both acne control and scar prevention. If not treated quickly, cystic acne can cause scars that are often harder to treat than the acne itself. Patients with cystic acne should see a board-certified dermatologist, like Dr. Michele Green in NYC, as soon as possible to stop breakouts and prevent scars.

Acne treatment – 1 and 6 months after.
Should you pop cystic acne pimples?
No! While it may be tempting to pop a cyst, it should be avoided because popping can lead to other complications. Cystic acne forms deep within the skin, preventing the lesion from reaching the surface, which makes it nearly impossible to manually extract the cyst by popping. Trying to pop a cystic acne lesion can cause inflammation, permanent skin damage, and the formation of scars that are often even harder to treat than the acne itself. Additionally, popping a cyst can introduce a serious infection and may result in cystic acne scarring. Instead of attempting to pop cystic acne lesions, consult a board-certified dermatologist, such as Dr. Michele Green in New York City, to develop a personalized treatment plan that includes prescription medications and in-office procedures to help clear your skin.
What is the best skincare product to treat cystic acne?
The foundation of an effective cystic acne routine begins with choosing the right cleanser. Gentle cleansers formulated with salicylic acid, glycolic acid, or benzoyl peroxide help clear pores, control excess oil, and prevent new breakouts. These ingredients target acne at its root without being too harsh, making them suitable for daily use. For those with sensitive skin, a mild foaming or cream-based cleanser can provide balance without stripping essential moisture.
After cleansing, targeted treatments are essential for managing cystic breakouts. Topical retinoids help regulate cell turnover and keep pores clear, while medicated pads or gels containing salicylic acid or benzoyl peroxide can be applied directly to active spots. Adapalene (Differin gel) and tretinoin (Retin-A), along with other topical retinoids, are derived from vitamin A and are commonly used to treat inflammatory and cystic acne. Azelaic acid is another topical option for cystic acne, known for its anti-inflammatory properties that help reduce cystic acne and improve hyperpigmentation caused by breakouts. These treatments penetrate deeply into the skin, reducing inflammation and speeding up healing, which is crucial for minimizing scarring. However, individuals with sensitive skin may find retinoids difficult to tolerate, as they can cause dryness and irritation.
To promote healing, keeping skin properly hydrated is key. A lightweight, non-comedogenic moisturizer helps strengthen the skin barrier, prevents irritation from active treatments, and balances oil production. This is especially important if you’re using products with active ingredients like salicylic acid, benzoyl peroxide, or retinoids, which can cause dryness. Lotions containing calming ingredients, such as niacinamide or ceramides, are particularly effective in reducing redness and irritation.
Ultimately, sunscreen is vital for protecting against UV damage and preventing dark marks from worsening. Broad-spectrum, oil-free SPF is ideal for acne-prone skin, as it provides protection without clogging pores and helps maintain an even skin tone. Since many active ingredients are potent on their own, consulting with a dermatologist ensures that the right products are combined safely and effectively, helping patients avoid unnecessary irritation while achieving optimal results. When you consult with Dr. Green at her private dermatology office in Manhattan’s Upper East Side, she will collaborate with you to develop a personalized skincare routine with specifically formulated products best suited for your skin type.
How to Prevent Acne Scars
Cystic acne develops deep beneath the skin, making it the most likely to leave permanent scars. The best way to prevent scarring is to treat breakouts early and avoid picking or squeezing lesions, which can drive bacteria deeper and worsen inflammation. Gentle skincare, including non-irritating cleansers and consistent sun protection, helps the skin heal more evenly and reduces the chances of lasting marks. For painful cysts, in-office treatments like corticosteroid injections can quickly decrease swelling and prevent tissue damage. Oral or topical medications prescribed by a dermatologist can also help control inflammation and stop cysts from progressing to a stage where scarring happens. Taking a proactive approach with the right treatment plan not only clears current breakouts but also helps maintain the skin’s texture and overall health over time.
How to get rid of cystic acne scars
Cystic acne is the most likely type of acne to cause scarring because it is highly inflammatory. The inflammation associated with acne lesions can cause permanent damage to skin tissue, leading to scars that are often more challenging to treat than the acne itself. Dr. Green is an expert in creating personalized acne scar treatment plans for patients, using advanced technologies and innovative techniques to help restore confidence by providing smooth, clear, and radiant skin that lasts. Whether the treatment involves laser skin resurfacing with Fraxel or eMatrix, subcision with dermal fillers, microneedling, or a combination of methods, Dr. Green aims to help you look and feel like the best version of yourself.
The Fraxel Dual laser is a non-invasive skin resurfacing treatment that uses two different wavelengths to improve the skin’s appearance. The 1550nm Erbium laser targets acne scars, fine lines, wrinkles, uneven skin texture, and large pores, while the 1927nm Thulium laser focuses on sun damage and pigmentation. This laser works by delivering fractionated energy to the deeper layers of the skin, stimulating collagen production to smooth the skin and reduce the visibility of scars. There is minimal downtime, with most patients experiencing mild redness, similar to a sunburn, for up to 48 hours. Typically, patients require a series of three to five sessions, each spaced approximately one month apart, to achieve optimal results with their acne scars.
The eMatrix laser is a resurfacing device that improves the look of acne scars and enhances skin texture. It uses radiofrequency energy to gently heat the deeper layers of the skin, stimulating the production of new collagen for a smoother appearance. Similar to the Fraxel laser, patients usually experience only mild redness for up to 48 hours after treatment. The eMatrix laser is safe and effective for all skin tones, including those with darker skin, making it an excellent option for treating acne scars. Several sessions, spaced one month apart, are needed to achieve optimal results.
Dermal fillers are a popular treatment option for acne scars because they effectively reduce the appearance of depressed scars. These fillers work by restoring lost volume, smoothing the skin, and reducing the appearance of acne scars. Products like Juvederm and Restylane contain hyaluronic acid, a naturally occurring substance in the body that attracts and retains moisture in the skin. Sculptra contains poly-L-lactic acid, which stimulates new collagen production for a smoother complexion. Dr. Green often performs subcision to break up the scar tissue beneath the skin, allowing for more effective cosmetic results. Hyaluronic acid fillers typically last for nine to twelve months before additional treatment is required, while Sculptra can last up to two years after a series of treatments.
Microneedling, also known as collagen induction therapy, is a non-invasive treatment that enhances acne scars, improves skin texture, reduces fine lines and wrinkles, and minimizes the appearance of pores. It utilizes tiny, surgical-grade needles to stimulate the body’s natural healing process and promote the growth of new collagen. Because the procedure enhances absorption of topical products, Dr. Green can pair microneedling with a depigmentation serum to treat post-inflammatory hyperpigmentation from previous cystic acne. Additionally, Dr. Green may utilize platelet-rich plasma (PRP) to accelerate healing and optimize results. PRP, made from a patient’s blood, contains proteins and growth factors vital for tissue repair. Patients usually need a series of at least three microneedling sessions to achieve optimal improvement in acne scars.
How to treat cystic acne at home (home remedies)
While many individuals and websites claim that homeopathic remedies can cure cystic acne, the most effective treatment comes from consulting a board-certified dermatologist, such as Dr. Michele Green. Cystic acne lesions develop deep within the skin and generally do not respond to topical treatments or home remedies. It is essential to address cystic acne promptly and professionally, as these lesions have a high likelihood of leaving permanent scars. Acne scarring often results from cystic acne breakouts due to the severe inflammation associated with cysts, which damages the skin tissue beyond its ability to heal. As a result, this can create areas of depressed skin connected by bands of scar tissue. To actively prevent the formation of acne scars and to clear cystic acne quickly, safely, and effectively, it is crucial to always consult a board-certified dermatologist. They can promptly diagnose your skin condition and recommend an appropriate combination of medications, topical skincare products, and in-office treatments to help you achieve a lasting, blemish-free complexion. However, Dr. Green offers treatments for those who want to improve the appearance of acne scars, including dermal fillers, Fraxel, eMatrix, and microneedling.

5 months before and after Acne treatment
Frequently Asked Questions (FAQs) about Cystic Acne Treatment
What is the lifespan of a cystic pimple?
Cystic pimples tend to last much longer than other types of acne. While small pimples, such as whiteheads or pustules, may clear within a few days, cystic lesions can persist for weeks or even months if left untreated. Because they form deep under the skin and cause significant inflammation, they do not surface easily and are less likely to heal on their own. In fact, many cysts rupture beneath the skin, increasing the risk of permanent scars. Prompt treatment by a board-certified dermatologist, such as corticosteroid injections or prescription medications, is the best way to reduce a cyst’s duration and prevent long-term skin damage.
Is cystic acne hormonal or bacterial?
Various factors, including hormonal and bacterial elements, can cause cystic acne. Hormonal acne usually appears during puberty, pregnancy, menopause, and menstruation. In adults, hormonal cystic acne often shows up along the jawline, but it can also affect the back, chest, neck, shoulders, and buttocks. Androgen hormones, such as testosterone, control sebum production. When androgen levels are out of balance, the skin’s oil glands produce too much sebum, which clogs pores and causes cystic acne to develop. Additionally, bacteria can become trapped in pores, resulting in inflammation, swelling, and the formation of acne cysts. To create the most effective personalized treatment plan for each patient with cystic acne, Dr. Green will carefully review your medical and family history and might request specific lab tests to identify the underlying causes of the breakouts.
How to treat hormonal cystic acne
Hormonal cystic acne, which is more common in females than males, often requires treatment with medications like spironolactone or birth control pills. Spironolactone (brand name Aldactone) helps regulate androgen levels to manage and prevent acne breakouts in women. Recently, the FDA has approved oral contraceptives to help women dealing with hormonal acne. Yaz, Ortho Tri-Cyclen, and Estrostep, containing both estrogen and progestin, are three commonly prescribed birth control pills for treating hormonal acne. Accutane, or oral isotretinoin, is another option that can effectively eliminate hormonal cystic or severe acne in a typical 20-week course. The first step in identifying the underlying causes of your cystic acne and resolving your breakouts is to consult a board-certified dermatologist with the expertise and experience needed to address your skin condition properly. Dr. Green in NYC has over 25 years of experience providing top-quality acne and acne scar treatments to patients worldwide. She will evaluate your skin condition and medical history to develop a personalized treatment plan tailored to your specific needs.
Will Accutane help eliminate cystic acne?
Yes! Accutane is the most effective medication for treating stubborn deep acne lesions, including cysts and nodules, that do not respond to any other oral or topical treatments. Accutane, or oral isotretinoin, is a vitamin A derivative that works by shrinking oil glands, reducing sebum production, and increasing skin cell turnover. After a short 20-week course, 95% of patients find that their acne is completely gone and do not experience any new breakouts or cysts. The remaining 5% of patients often need a second course of Accutane to clear their cystic acne. Accutane must be prescribed and closely monitored by a board-certified dermatologist. Patients are required to have monthly visits and blood tests to continue receiving the medication. Additionally, patients who could become pregnant must have monthly pregnancy tests and agree to abstain or use two methods of birth control, as taking Accutane during pregnancy can cause severe birth defects.
What triggers cystic acne?
Cystic acne develops when bacteria cause inflammation deep under the skin, leading to painful, pus-filled bumps. The development of cystic acne is largely influenced by genetics, but various external factors can also contribute to its onset. These triggers include fluctuating hormones (especially sex hormones and androgens), lack of sleep, high stress levels, poor hygiene, and diets rich in sugar, dairy, and fat. Moreover, people with oily skin are more prone to cystic acne because excess oil blocks pores.
Will doxycycline treat cystic acne?
Yes, doxycycline is a common oral antibiotic used to treat and clear up acne, including cystic acne. It’s essential to use proper sun protection when taking doxycycline or any other antibiotic, as the medication can increase the skin’s sensitivity to sunlight. Patients should apply a broad-spectrum sunscreen with an SPF of 50 and reapply it every two hours. They should also avoid sun exposure and wear sun-protective clothing, such as hats and sunglasses.
Does spironolactone help treat acne?
Yes, spironolactone is an oral medication that helps treat acne in women by blocking androgen activity, which is a male hormone. Androgen can increase oil production in the skin, often leading to clogged pores and cystic breakouts. By reducing this hormonal effect, spironolactone lowers sebum levels and helps prevent the formation of painful cysts and inflammatory acne. It is especially effective for women with hormonal acne that flares around the jawline, chin, or during their menstrual cycle. Spironolactone is not usually prescribed for men because of its anti-androgen effects, but for women, it can be a safe, long-term option under a dermatologist’s supervision. Since it primarily treats hormonal acne, it is essential to schedule a consultation with a dermatologist, such as Dr. Green, to determine the type of acne you have, allowing her to provide a treatment plan tailored to your specific condition.
Will tretinoin help improve cystic acne?
Tretinoin, commonly known by its brand name Retin-A, is an effective topical treatment for cystic acne. This vitamin A derivative helps regulate oil production and reduces inflammation. It also speeds up skin cell turnover, removing dead skin cells and impurities to clear clogged pores and prevent new breakouts. Tretinoin comes in various strengths and should be prescribed by a board-certified dermatologist, such as Dr. Michele Green. When using tretinoin, it is important to practice proper sun protection, as it can increase skin sensitivity to sunlight.
Will retinol help cystic acne?
Retinols are skincare products derived from vitamin A that accelerate skin cell turnover. Dead skin cells are shed more quickly than normal, revealing healthy new skin cells and keeping pores clear. In addition to reducing breakouts, retinol also boosts collagen production, improving the appearance of fine lines, hyperpigmentation, and other signs of aging. Unlike tretinoin, retinol does not require a prescription and can be bought over the counter. However, it is less potent than tretinoin or other prescription retinoids and might not effectively treat cystic acne. Dr. Green will work with you to customize your skincare routine to include products like retinol or prescription-strength retinoids that are best suited for your cystic acne, helping you achieve clear, acne-free skin.
Will salicylic acid help cystic acne?
Salicylic acid is an effective ingredient for combating cystic acne. As a beta-hydroxy acid, it binds to excess oil and impurities, breaking them down at a molecular level and releasing them from pores while gently exfoliating the skin. Additionally, salicylic acid reduces sebum production and accelerates cell turnover, effectively removing dead skin cells and preventing clogged pores.
Should I exfoliate cystic acne?
Exfoliation should be approached cautiously when dealing with cystic acne. Since cystic lesions form deep under the skin and are highly inflamed, harsh scrubs or frequent exfoliation can worsen irritation, increase redness, and raise the risk of scars. It is best to avoid abrasive scrubs and instead use gentle exfoliants such as glycolic acid (AHA) or salicylic acid (BHA), which help remove dead skin cells without causing physical damage. Over-exfoliating or scrubbing too aggressively can lead to increased oil production and slow down healing. For cystic acne, gentle exfoliation can support a skincare routine, but treatment from a dermatologist is usually necessary to fully clear breakouts.
Will benzoyl peroxide clear cystic acne?
Benzoyl peroxide reduces inflammation and kills acne-causing bacteria, which can be helpful for treating cystic acne. It is especially effective in managing inflammatory acne lesions, such as cysts, compared to other types like blackheads and whiteheads. Benzoyl peroxide is available in many over-the-counter cleansers and spot treatments. Before adding a benzoyl peroxide product to your skincare routine, consult with Dr. Green at her private dermatology office in NYC. Dr. Green will ensure that your skincare routine includes products suited to your specific skin type and condition.
Will steroid cream help cystic acne?
Steroid creams, such as hydrocortisone, can effectively reduce inflammation and redness associated with cystic lesions. They can also relieve pain caused by the cysts. However, topical creams are often ineffective for cystic acne because they don’t penetrate deep enough into the skin where the cysts form. To treat cystic acne, Dr. Green may inject corticosteroids into the cysts to reduce their size, decrease inflammation, and lower the risk of scarring.
Can diet affect cystic acne?
Yes, diet can affect cystic acne in some people. Research shows that high-glycemic foods, such as white bread, sugary drinks, and processed snacks, which quickly raise blood sugar levels, can trigger hormonal changes that increase oil production, leading to more breakouts. Dairy products, particularly skim milk, have also been associated with acne in certain individuals. While diet isn’t the only cause of cystic acne, reducing sugar intake and eating more whole, nutrient-rich foods may help support clearer skin.
What deficiency causes cystic acne?
There isn’t a vitamin or mineral deficiency proven to directly cause cystic acne, but research suggests that certain deficiencies may worsen breakouts. Low levels of vitamin D and zinc have been linked to more severe acne in some studies, as both support immune function and skin’s healing ability. For example, zinc deficiency can impair the skin’s healing process, while vitamin D helps boost immune defense against acne-causing bacteria. Omega-3 fatty acids, found in fish, walnuts, and flaxseeds, play a key role in reducing inflammation throughout the body. However, cystic acne primarily results from hormonal imbalances, genetics, excess oil production, and inflammation, rather than solely from nutrient deficiencies. Although current research suggests a possible connection, further studies are needed to understand how these factors affect cystic acne fully. Addressing dietary deficiencies or supplementing with specific nutrients might improve overall skin health, but it’s essential to consult a dermatologist for effective cystic acne management.
Which gut bacteria cause cystic acne?
Currently, no specific gut bacteria have been proven to directly cause cystic acne. However, research suggests that imbalances in the gut microbiome may contribute to inflammation and hormonal shifts that can exacerbate acne. Some studies have linked higher levels of certain bacteria, like Escherichia coli and other Gram-negative species, to skin inflammation. On the other hand, beneficial bacteria such as Lactobacillus and Bifidobacterium seem to reduce inflammation and support healthier skin. Additionally, experimental studies suggest that stress can disrupt the normal gut microflora, particularly Lactobacillus and Bifidobacterium species, indicating that lifestyle factors may contribute to cystic acne. While more research is necessary, maintaining a balanced gut microbiome through a healthy diet, probiotics, and lifestyle choices might help manage cystic acne.
Will pimple patches work on cystic acne?
A pimple patch is a hydrocolloid bandage that covers an inflammatory acne lesion, pulling out the excess sebum and oil clogged in the pores. Hydrocolloid bandages work to dry up surface-level pimples and pustules, and many pimple patches include additional acne-fighting ingredients to help reduce breakouts. While a pimple patch can effectively extract the contents of an acne lesion on the skin’s surface, it is not effective for treating cystic acne that forms deep beneath the skin. Applying a hydrocolloid bandage to a cyst may help shrink the lesion’s size; however, it is unlikely to eliminate a cyst. Consulting a board-certified dermatologist, such as Dr. Green, is the best way to manage cystic acne and prevent scarring.
Will Ibuprofen help cystic acne?
Over-the-counter pain relief medications, such as Advil and ibuprofen, can help alleviate tenderness and discomfort associated with cysts but will not directly treat them. Ibuprofen has anti-inflammatory properties that decrease swelling and relieve pain caused by pressure from the cysts. These pain relievers are not meant for topical use and should never be applied directly to a pimple. Instead, schedule an appointment with a board-certified dermatologist such as Dr. Green, who can accurately diagnose and treat your cystic acne.
Why am I getting cystic acne all of a sudden on my back?
Sudden cystic breakouts on the back can occur due to various factors, including hormonal changes, genetics, and lifestyle choices. Back acne often occurs when sweat, oil, and dead skin cells become trapped under clothing, a condition sometimes referred to as acne mechanica. Tight-fitting clothes and backpacks can increase friction and heat, clogging pores and causing inflamed cysts. Hormonal shifts from puberty, stress, or menstrual cycles can also raise oil production, worsening breakouts. Additionally, pore-clogging skincare or hair products that rub against the back can trigger flare-ups. Maintaining good hygiene, showering after sweating, using non-comedogenic products, and wearing looser, breathable clothing can help prevent future outbreaks. However, severe or persistent cystic acne may require professional treatment.
How to treat cystic acne while pregnant
It is common for women to experience cystic acne breakouts during pregnancy due to increased hormone levels, including androgens. These hormones can affect sebum production in the skin, leading to excess oil, clogged pores, and cystic acne lesions. It is crucial to exercise caution when using skincare products and medications during pregnancy to protect both the mother and the developing fetus. Medications such as retinoids and antibiotics can potentially cause birth defects and should be avoided during pregnancy. Additionally, Accutane should not be prescribed when pregnant, as it can cause severe congenital defects in the fetus. If you choose to breastfeed, many of these same medications should still be avoided because their effects can potentially pass to your infant. It is essential to consult with your obstetrician or dermatologist before starting any topical or oral medications to ensure they are safe for both you and your baby.
How to bring cystic acne to a head?
Unlike whiteheads or pustules, cystic pimples develop deep beneath the skin and rarely form a visible “head.” Because they are trapped below layers of tissue, trying to squeeze or pop them will not bring the contents to the surface and can often worsen inflammation and scarring. Dermatologists may use procedures such as corticosteroid injections to quickly reduce swelling or perform acne surgery to drain a lesion when needed, all while being careful. At home, applying warm compresses can sometimes ease discomfort and promote slight drainage, but cystic pimples generally require professional treatment for complete removal.
What is stage 4 cystic acne?
Dermatologists typically classify acne into four stages, from mild blackheads and whiteheads to severe cystic breakouts. This classification helps evaluate the severity of acne and guides the best treatment options. Stage 4 acne is the most advanced form of acne vulgaris, marked by widespread, deep, and painful nodules and cysts. Unlike earlier stages, which may include blackheads, whiteheads, or occasional inflamed pimples, stage 4 often affects large areas of the face, back, chest, or shoulders with inflamed lesions that can merge. Due to the intense inflammation and depth of the cysts, this stage carries the highest risk of permanent scarring if left untreated. Managing stage 4 acne generally involves prescription oral medications, such as isotretinoin, and might also include in-office procedures to minimize scarring and prevent long-term damage.
What makes cystic acne worse?
Several factors can worsen cystic acne. Not washing the skin after aerobic exercise can make cystic acne worse because sweat can trap dead skin cells, debris, and bacteria in the pores. Overwashing or scrubbing too hard can also aggravate cystic acne by stripping the skin of its natural oils, which causes the body to produce excess oil in response. Using skincare products that are not suitable can further inflame cystic acne, especially if the products contain oils or tend to clog pores. Picking your skin or squeezing your acne breakouts can make cystic acne worse. It’s essential to select your skincare products carefully and adjust your routine to prevent exacerbating your acne, inadvertently increasing sebum production, or irritating your skin. When you visit Dr. Michele Green’s office in New York City, she will discuss the best combination of skincare products, procedures, and acne medications to help you clear your cystic acne as quickly, safely, and comfortably as possible.
How do I get started with cystic acne treatment today?
Cystic acne can be painful, cause scarring, and lead to feelings of self-consciousness or low self-esteem for many people. Cysts are a severe type of inflammatory acne that forms deep within the skin. Unlike pimples, whiteheads, and blackheads, cysts typically do not respond to topical treatments and, if left untreated, can lead to permanent skin damage and scarring. Instead of trying various over-the-counter options with little success, schedule a consultation with a board-certified dermatologist like Dr. Green, who will work with you to develop a personalized acne treatment plan based on your skin type and the specific type of acne you have. Dr. Green often recommends a combination of in-office procedures, oral medications, and targeted skincare products to help you achieve and maintain a smooth, clear, and healthy complexion that lasts.
Dr. Michele Green is a highly respected, board-certified dermatologist with over 25 years of experience helping some of the world’s most discerning individuals. She provides optimal treatment options for active cystic acne breakouts and residual scars. Thanks to her dedication and expertise, Dr. Green is repeatedly recognized as one of NYC’s top dermatologists by Castle Connolly, Super Doctors, New York Magazine, and The New York Times. She takes a holistic approach to acne treatment, personalizing each patient’s plan with a combination of skincare products, in-office procedures, topical treatments, and oral medications tailored to individual needs and goals. To learn more about how cystic acne develops and to start treatment with Dr. Green, please contact us online today or call our dermatology office based in New York City at 212-535-3088.
 212-535-3088
212-535-3088