Back Acne
Back acne, commonly referred to as “bacne,” is one of the most common types of acne, affecting more than half of all individuals who experience breakouts. According to the American Academy of Dermatology (AAD), over 50 million Americans deal with acne each year, making it one of the most common skin issues. It can occur anywhere on the body, often causing patients to feel self-conscious. When it appears on the back, it usually presents as cysts or nodules, which can be painful and uncomfortable. Back acne can affect people of any age and gender, with risk factors including poor hygiene, an inadequate skincare routine, high stress levels, and a family history of acne. Managing acne treatment and prevention can be overwhelming, so consulting a board-certified dermatologist, such as Dr. Michele Green in NYC, is essential. Dr. Green specializes in treating all types of acne, including back and facial acne, and can help you achieve clear, healthy skin by permanently removing back acne.
Several treatment options and preventive strategies can be used to treat back acne and prevent future outbreaks. Prevention might be as simple as changing your post-workout bathing routine or washing your linens more frequently. When these steps aren’t enough, many over-the-counter topical cleansers and creams containing benzoyl peroxide or salicylic acid are available to help remove dead skin cells, clear pores, and reduce acne. If these topical treatments don’t work, it’s time to see Dr. Green to explore other options, such as HydraFacials, prescription medications like oral antibiotics, or Isotretinoin (Accutane). Dr. Green can also help you develop a personalized skincare routine with the best products to keep your skin clear and smooth.
Dr. Michele Green is an internationally acclaimed, board-certified dermatologist specializing in cosmetic dermatology with over 25 years of experience. She offers some of the most discerning men and women worldwide the best non-invasive treatments for acne and acne scars. At her private dermatology practice on the Upper East Side of Manhattan, she skillfully uses the latest technology and innovative techniques to provide natural-looking, long-lasting results that help her patients look and feel their best. She is consistently recognized as one of New York’s top dermatologists by Super Doctors, New York Magazine, and Castle Connolly. When working with Dr. Green, she recommends a personalized blend of premium skincare products and in-office treatments, such as Botox, dermal fillers, chemical peels, laser therapies, and more, to achieve optimal results.
What is back acne (bacne)?
Back acne, also known as “bacne,” is a common breakout that appears on the back. While the face is the most common area for acne, it can develop anywhere on the body where sebaceous glands are present. Body acne, which often appears on the chest, back, and buttocks, can be frustrating and uncomfortable for many individuals. Back acne is most often found along the shoulders and upper back, but can occur anywhere on the back. It can include whiteheads, blackheads, pimples, papules, cysts, or nodules. Although hormonal changes like puberty or pregnancy are common causes, anyone can develop bacne. Factors like genetics, lifestyle, medications, skincare, and hygiene also play a role. Prompt and effective treatment is crucial to prevent long-term scarring, which can be more difficult to treat than the acne itself. Therefore, consulting a board-certified dermatologist, such as Dr. Michele Green in NYC, as soon as possible, is essential for proper care.
What are the different types of acne?
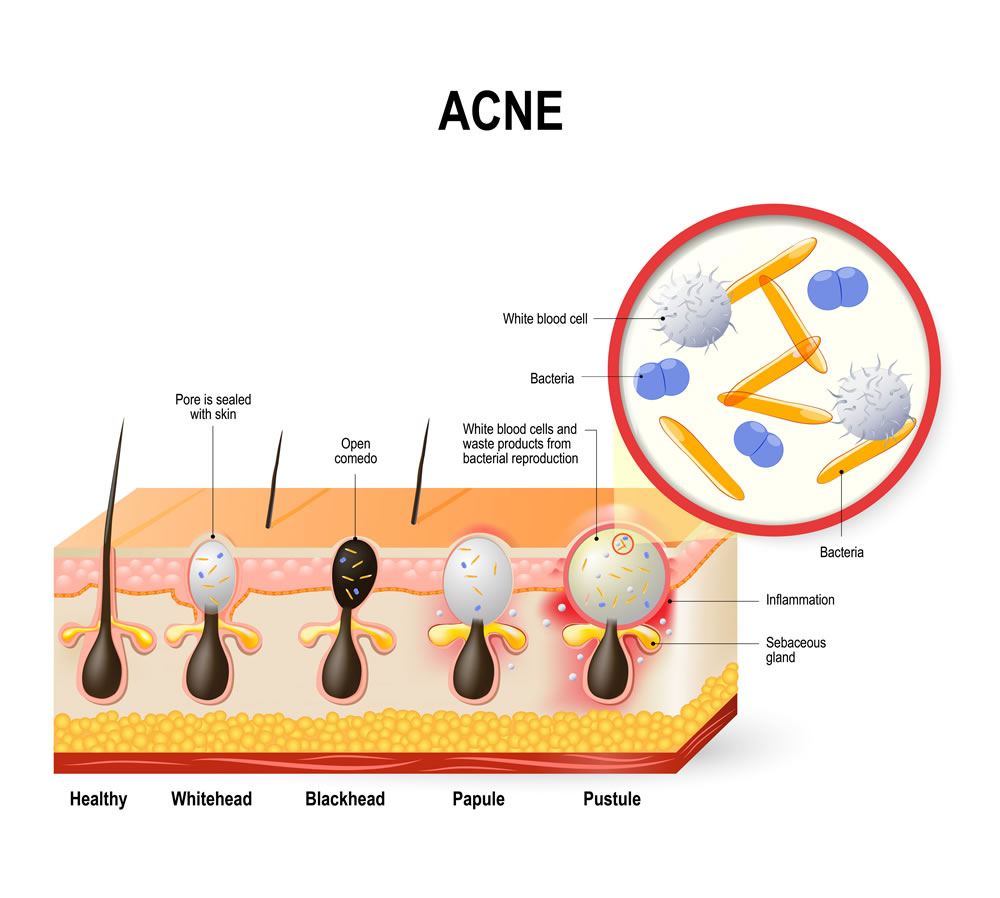
Several types of acne lesions can develop on the back, including whiteheads, blackheads, papules, pustules, nodules, and cysts. Whiteheads, also called closed comedones, form when pores or hair follicles become clogged with dirt, debris, and sebum. They are called closed comedones because the pore remains shut, trapping debris beneath the skin and giving the bump a white top. Similarly to whiteheads, blackheads form when oil, dead skin cells, and other debris clog the hair follicle. However, unlike whiteheads, blackheads are open comedones, meaning that the pore is open on the skin’s surface. The open comedones appear black due to the reaction of sebum in the pore with the air.
Papules are a type of inflammatory acne that appear as red bumps on the skin’s surface. They may be painful or irritated, but they do not have a pus-filled tip. Pustules, often referred to as pimples, are another type of inflammatory acne. Unlike papules, pustules are filled with pus caused by an accumulation of white blood cells. The pus often gives pustules a white or yellow appearance. Nodules form when a clogged hair follicle becomes infected with bacteria. They can develop deeper within the tissue, resulting in a hard, red bump on the skin’s surface that is often painful. Cystic acne occurs when pus-filled acne is also infected with bacteria. Cysts form deeper under the skin and often develop a red bump on the surface, causing pain and discomfort.
What is the cause of back acne?
Acne occurs when excess oil, dead skin cells, sweat, and other debris clog the skin’s pores. Clogged pores can cause the oil glands, known as sebaceous glands, to produce more sebum, which can worsen the buildup of debris in the follicles. Sometimes, when pores are blocked, skin bacteria called cutibacterium can become trapped inside, leading to inflammation and more painful pimples. The pores on the back are especially prone to sweat acne, which can happen when sweat, friction, and heat combine to clog pores and trap cutibacterium within them. Friction from backpack straps, sports gear, non-wicking clothing, hats, and headbands can also contribute to this issue. Luckily, simple lifestyle changes can help reduce the risk of developing back acne.
Why do I have back acne?
Many factors contribute to the development of back acne, including:
Genetics: Patients with a family history of acne are more likely to experience breakouts than those without. Moreover, individuals with a genetic predisposition to increased sebum production are at a higher risk of clogged pores due to excessive oil.
Hormone Fluctuations: Changes in hormone levels can also lead to breakouts of bacne. People experiencing puberty, menstruation, or pregnancy may be more prone to body acne due to hormone fluctuations during these times.
Poor Hygienic Practices: You may be more prone to developing zits on your back if you don’t practice proper hygiene. After exercising or any activity that causes sweating, sweat trapped under workout clothes can clog pores, trapping oil, dirt, and debris, which can worsen existing acne or lead to new breakouts. Sweat left on the skin can harbor bacteria, causing breakouts. Additionally, if you don’t wash your sheets and pillowcases regularly, dirt, dead skin cells, and debris can remain on the surface and clog pores.
Diet: Diets high in the glycemic index, which are rich in carbohydrates and sugars, can lead to acne breakouts. Foods that raise your blood sugar levels, such as bread, sugary pastries, cereals, milk, and soda, can also increase the chances of bacne. Cutting back on these types of foods may help decrease acne.
Friction: Acne mechanica is a type of acne that is more likely to develop when friction occurs between clothing or equipment and the skin. This type of acne is especially exacerbated when sweat is present in the area. For example, back acne breakouts often tend to form where the shoulder straps of a backpack rub against the back. Similar breakouts can happen when there is close skin contact with other sports equipment or tight clothing.
Medication: Some prescription medications can increase your likelihood of developing body acne, including corticosteroids, progestin contraceptives, lithium, and more.
Improper skin care: Certain skin care products, such as some lotions and creams, may have a high oil content and can, therefore, contribute to the production of excess sebum, which can clog your pores. Patients with acne-prone skin should ensure that their skincare products are labeled as non-comedogenic, meaning they will not clog pores. Some patients with back acne may scrub their backs to exfoliate, but instead of clearing bacne, the friction can actually exacerbate the condition by irritating the skin.
Stress: Patients who face a stressful environment or anxiety may be more prone to developing acne breakouts all over their bodies. Stress can cause an overproduction of certain hormones, which can increase the production of sebum from oil glands. This excess sebum can clog pores, leading to acne and other breakouts.
How do you treat back acne?
When navigating the many treatment options for back acne, it is best to begin by consulting a board-certified dermatologist, such as Dr. Green. One of the most important reasons to consult with an experienced board-certified dermatologist as soon as possible regarding your back acne is that inflammation associated with acne lesions can cause acne scars to form. Acne scars are often much more difficult to treat than acne breakouts themselves. Treating acne effectively and immediately is the best course of action for preventing acne scars. Dr. Green can help determine the combination of oral medications, skincare products, in-office procedures, and topical treatments that will work best for your type of acne and lifestyle. When you consult with Dr. Green, you will have the opportunity to discuss your specific skin concerns and overall aesthetic goals. She will then work with you to create a customized treatment plan tailored to your needs.

What is the best skincare for back acne?
Cleansers and exfoliators for acne
Cleansing the skin is a crucial step in any acne skincare routine. Using a cleanser or body wash regularly helps reduce the buildup of dead skin cells, oil, dirt, sweat, and other impurities, preventing pores from clogging. Glycolic acid and salicylic acid, two hydroxy acids, work together to gently exfoliate and dissolve excess oil, treating and clearing your acne. The Pore Minimizing Cleanser from MGSKINLABS, Dr. Green’s proprietary skincare line, contains both glycolic and salicylic acid to clean pores and help prevent acne breakouts thoroughly.
Exfoliation is the process of removing dead skin cells and other impurities from the skin to clear pores and reveal fresh, healthy skin underneath. Patients can use an exfoliant two to three times a week or as needed to prevent bacne. The Retexturizing Pads from MGSKINLABS contain glycolic and salicylic acid to provide an at-home peel effect, exfoliating dead skin cells and preventing pore blockages to help stop acne.
Acne spot treatments
Spot treatments are made with strong acne-fighting ingredients to target and eliminate active blemishes. Many include benzoyl peroxide, an antibacterial agent that kills the bacteria responsible for causing acne. MGSKINLABS’ Acne Spot Treatment contains 5% benzoyl peroxide and can be used as needed to reduce oil production, decrease inflammation, and shrink pimples.
Moisturizer
Regardless of skin type, a moisturizer is an essential component of any skincare routine, particularly for individuals with oily or acne-prone skin. While most people believe acne only occurs on oily skin, it can also happen on dry skin due to the body’s overproduction of sebum. Light, oil-free moisturizers are essential for acne-prone skin, as they help keep the skin hydrated while preventing clogged pores. MGSKINLABS’ Ultimately Sheer Hydrating Lotion is ideal for individuals with sensitive skin, as it helps control oil production, reduces excess sebum, and leaves a matte finish, making it perfect for those with acne-prone skin.
Sunscreen
Another essential part of a good skincare routine is using sunscreen. Choosing a non-comedogenic sunscreen is ideal for those with oily or acne-prone skin. Dr. Green’s MGS, Inc. offers a non-comedogenic Hydrating SPF 50 that combines a moisturizer and SPF into one product. This type of sunscreen is ideal for individuals who want to maintain their skin’s hydration and radiance while protecting against UV rays that can lead to skin cancer and premature aging. Sunscreen should be reapplied every 90 minutes or after any water activities.
Dermatologist-approved back acne treatments
There are many ways to approach reducing back acne, including prescription topicals, oral medications, and in-office procedures. Although acne is an incredibly common skin condition, every individual may break out for different reasons. Thus, each patient requires a customized acne treatment plan to appropriately and effectively clear their breakouts. The first step in eliminating back acne blemishes is to consult with an experienced dermatologist, such as Dr. Green in NYC. With over two and a half decades of experience, Dr. Green will examine the type of acne you are dealing with and recommend the best course of action to treat your acne.
Acne surgery
Acne surgery is an in-office procedure used to treat inflammatory acne lesions, including papules, pustules, and cysts. During the procedure, active acne lesions are opened, and their contents—such as dead skin cells, dirt, and sebum—are removed with a medical tool. A steroid is then injected into the area to decrease inflammation and shrink the lesion. Acne surgery is highly effective at eliminating breakouts and significantly reduces the risk of acne scarring after healing.
VBeam laser
The VBeam laser is a 595nm pulsed dye laser that reduces red pigmentation in the skin. It is an effective treatment for acne because it decreases inflammation and eliminates acne-causing bacteria from the skin’s surface. There is no downtime with this treatment, and patients can resume their daily activities immediately afterward. In addition to treating acne, the VBeam laser also targets red acne scars, post-inflammatory hyperpigmentation, rosacea, facial redness, broken capillaries, and red stretch marks. Patients may need three to six treatment sessions, spaced one month apart, to achieve optimal acne results.
HydraFacials
A HydraFacial is a three-step medical-grade hydra dermabrasion treatment that gently cleanses, exfoliates, and nourishes the skin. Its proprietary vortex technology effectively removes sebum, dead skin cells, and debris trapped in the pores that cause acne. After cleansing and exfoliating, antioxidants, vitamins, and peptides are infused into the skin to boost its natural protective barrier. The treatment can also be combined with LED light therapy and specialized boosters to target specific skin concerns, including acne. The red LED light helps reduce redness and inflammation associated with acne, while the blue LED light kills acne-causing bacteria on the skin’s surface. Boosters are applied after cleansing and exfoliating to deliver targeted active ingredients. The Murad Clarifying Booster offers a deeper pore cleanse to reduce breakouts, while the ZO Rozatrol Booster helps lessen redness and inflammation. HydraFacial can be performed on various areas of the body prone to acne, such as the face, back, and buttocks. Typically, patients receive an initial series of three HydraFacials spaced one month apart, followed by maintenance treatments as needed to improve the results.
Chemical Peels
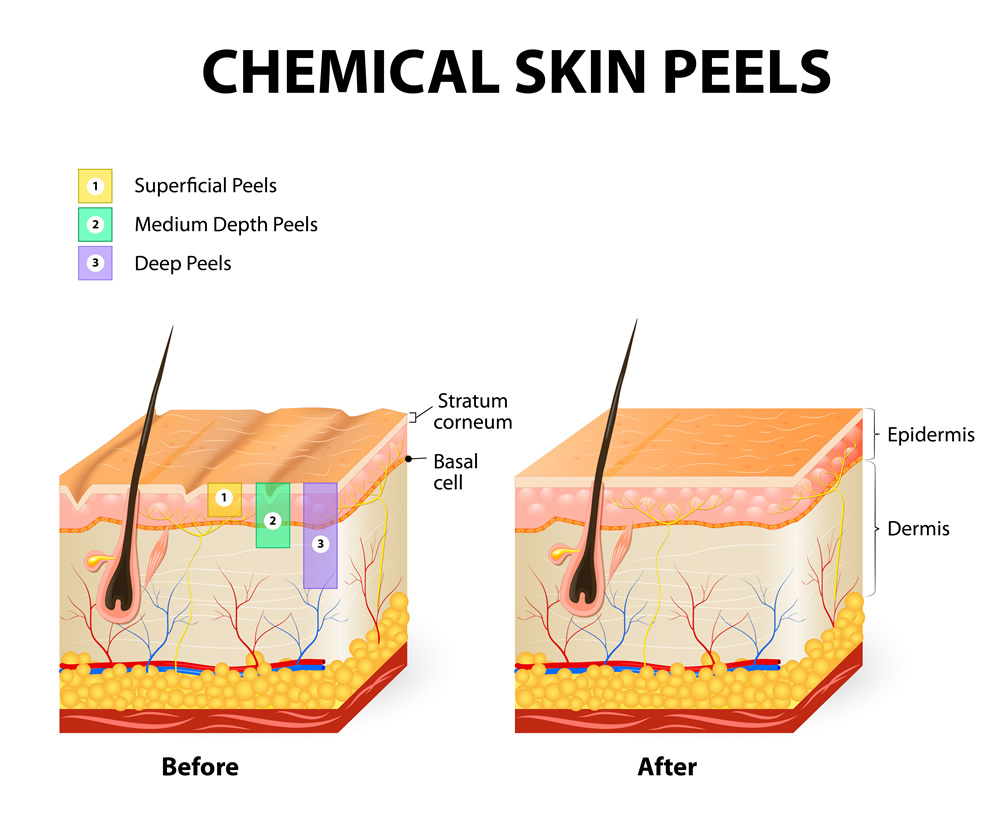
A chemical peel is a non-invasive cosmetic treatment that boosts skin cell turnover, removing dead skin cells from the surface and unclogging pores. Chemical peels help treat acne and also improve dullness, fine lines, and uneven skin tone. There are many types of chemical peels available, and Dr. Green works with each patient individually to tailor their treatment to their unique needs and aesthetic goals. Multiple sessions spaced three to four weeks apart are usually necessary to achieve the best results.
Oral medications
Oral antibiotics are an effective treatment for acne because they help lower the bacteria that cause breakouts on the skin’s surface. Commonly prescribed oral antibiotics for acne include Minocycline, Tetracycline, and Doxycycline. However, oral antibiotics should not be used as a long-term solution.
Women experiencing back acne can consider Spironolactone, an oral androgen blocker that regulates androgens, such as testosterone, to reduce sebum production and prevent breakouts. Oral contraceptives can also be effective against acne due to estrogen and progestin. Ortho Tri-Cyclen, Yaz, and Estrostep are three FDA-approved oral contraceptives for treating acne.
Patients with moderate to severe cystic or nodular acne, or those experiencing persistent acne breakouts that do not respond to other treatments, may consider oral isotretinoin. Isotretinoin, commonly known as Accutane, is a vitamin A derivative that reduces sebum production, levels of acne-causing bacteria, and inflammation, helping to eliminate acne breakouts permanently. Accutane also speeds up skin cell turnover, preventing dead skin cells from clogging pores. It is usually prescribed for a short course, typically 5 to 6 months. Patients on Accutane are required to have monthly visits and blood work with Dr. Green to continue their treatment. Women must also commit to abstinence or use two forms of birth control during treatment. Approximately 95% of patients who take Accutane achieve permanent clearance of their acne; the remaining 5% may require a second course for complete clearance.
Topical treatments
Topical antibiotics are very effective at reducing the prevalence of acne-causing bacteria on the skin. Commonly prescribed topical antibiotics include erythromycin and clindamycin. Winlevi is a topical treatment that contains clascoterone, an androgen blocker that inhibits the skin’s production of excess sebum. Topical retinoids are often prescribed for acne on the back. Like oral isotretinoin, topical retinoids are vitamin A derivatives that speed up skin cell turnover, reduce inflammation, and prevent clogged pores. Commonly prescribed retinoids include tretinoin and tazarotene.

How do I stop my acne from coming back?
Apart from in-office treatments, oral medications, and topical prescription creams, patients can also make lifestyle changes to reduce the risk of developing bacne. One way to prevent back acne is to improve your hygiene habits, especially around workouts and activities that cause sweating. Patients should wear moisture-wicking, loose-fitting clothing during exercise to reduce the amount of sweat trapped on the skin’s surface. It is also important to shower as soon as possible after working out to wash away any remaining sweat and help prevent clogged pores. If showering immediately isn’t possible, using cleansing wipes to remove sweat before changing out of dirty workout clothes is recommended. Reducing friction can also help prevent breakouts on the back. Instead of wearing a backpack, try an over-the-shoulder or rolling bag to lessen the friction caused by strap contact. Mental and emotional health is also essential for overall wellness. Stress can lead to hormone imbalances, which may increase sebum production. Whenever possible, find ways to reduce stress and anxiety to lower the chances of acne breakouts.
In some cases, acne breakouts on the back will resolve naturally over time. By making certain adjustments to hygiene and lifestyle practices, patients can maintain clean skin, which may help reduce back acne breakouts. If, however, severe acne persists despite following recommended skincare and hygiene routines, it is best to consult a board-certified dermatologist. An experienced dermatologist, such as Dr. Green in NYC, can identify the root causes and recommend the most effective treatment options for your skin.
Will back acne result in scarring?
When acne breakouts are left untreated, there is a risk that inflammatory lesions can irreparably damage the underlying skin tissue, leading to permanent acne scars. These scars are much harder to treat than the acne itself and can appear as either hypertrophic (raised) or atrophic (depressed) scars. Most acne scars won’t disappear on their own because they result from permanent damage to the skin. However, various non-invasive cosmetic treatments can significantly improve the appearance of acne scars, restoring an even, smooth skin texture and enhancing self-confidence. The first step in addressing acne scars is to schedule an appointment with a board-certified dermatologist, such as Dr. Michele Green in NYC, to identify the most effective treatment for your skin type, tone, and the specific scars you have.
How to treat back acne scars
One of the main reasons to see a dermatologist promptly for your acne breakouts is to prevent acne scars. Acne scars form when inflammation from the lesions causes permanent damage to the skin beneath. Although more difficult to treat than active acne, there are options for scar treatment. The V-Beam, eMatrix, and Fraxel lasers, as well as chemical peels, are among the most effective treatments available at the office of board-certified dermatologist Dr. Michele Green for improving the appearance of back acne scars and reducing redness. When you consult with Dr. Green about your back acne or scars, she will work with you to create a personalized treatment plan based on your specific needs.
The V-Beam laser is considered the gold standard for treating redness, including that caused by acne scars. It uses pulsed dye light energy, which is transformed into heat and absorbed by the red pigment in the skin, leaving the surrounding tissue unharmed. The V-Beam laser is effective for various skin types, including sensitive skin, and is suitable for both atrophic and hypertrophic scars. It can also improve the appearance of broken blood vessels, rosacea, and stretch marks, among other concerns. The procedure is quick, involves minimal downtime, and is generally painless.
The Fraxel Dual laser is considered one of the most effective options for treating atrophic acne scars. Fraxel uses two different wavelengths, 1550 nm and 1927 nm, to target both uneven skin texture and tone. While the surface layers of the skin remain intact, the middle layers receive controlled, microscopic injuries that stimulate the skin’s natural healing process, encouraging the production of new collagen and elastin. When using the 1550 nm setting, patients can expect less visible acne scars and clearer, smoother skin. The most common side effects are usually mild, such as inflammation or redness, which typically last for the first 48 hours after treatment.
The eMatrix laser is a popular choice for treating acne scars and is safe for patients of all skin tones and types. It utilizes radiofrequency technology to heat deep into the dermis, triggering the skin’s natural healing process and promoting collagen remodeling and the growth of new collagen. This new collagen helps create a smoother skin texture and diminishes the appearance of acne scars. The eMatrix laser has minimal downtime, with common side effects such as redness and peeling in the treated area, which typically last up to 48 hours.
Chemical peels are a skin resurfacing treatment that applies a peeling agent to remove the top layers of skin, helping to eliminate dead skin cells and blemishes, boost new collagen production, and uncover healthier skin underneath. They can be used to address unwanted pigmentation, active acne, and scars. Dr. Green will customize your chemical peel to ensure you get the best results.
Mesopeels are specialized chemical peels designed to treat hyperpigmentation and post-inflammatory inflammation. Some patients may notice dark spots remaining after an acne lesion has healed, and these spots form due to increased melanin production in the affected area. Mesopeels use skin-lightening agents, including kojic acid, azelaic acid, and tranexamic acid, to reduce unwanted hyperpigmentation and inhibit melanin production. They are safe for all skin types and tones and can be applied to various areas of the body, including the back, face, chest, inner thighs, and groin.
FAQs On Back Acne:
What type of acne is back acne?
There are many types of acne, and any of these can occur on the back. Some patients may experience a combination of blackheads, whiteheads, pustules, papules, cysts, and nodules. When seeking treatment for back acne, it is essential to consult a qualified dermatologist who can recommend the most suitable treatment for your specific type of acne.
Where do back pimples come from?
Several factors can contribute to back acne, including both biological and lifestyle factors. Biological factors might include family history or hormonal changes. Lifestyle factors encompass hygiene, skincare routines, diet, medication use, and stress levels. Maintaining good hygiene and a proper skincare routine can significantly reduce the risk of developing bacne. Behaviors that may contribute to it include wearing tight clothing, not showering immediately after workouts, not washing clothes between exercises, and eating a diet high in foods with a high glycemic index. Adopting habits that maintain skin cleanliness and health can significantly reduce the likelihood of developing acne.
Is back acne normal during pregnancy?
Pregnancy acne is very common, with over fifty percent of pregnant women developing it, usually starting around the sixth week of pregnancy. During the first trimester, your body produces more of the hormone progesterone, which increases the production of sebum—the oil produced by the sebaceous glands that lubricates the skin and hair. While sebum production is a natural process, excess oil can clog pores, leading to acne outbreaks or exacerbating existing acne. Therefore, pregnancy itself does not directly cause acne; however, hormonal changes during pregnancy can lead to skin alterations that often result in the development of acne. A history of acne or flare-ups at the start of your menstrual cycle is another risk factor for developing acne during pregnancy. To help manage back acne during pregnancy, it’s essential to follow a consistent skincare routine, avoid harsh chemicals, and consult with an experienced dermatologist for personalized advice to keep your skin clear and healthy.
Is back acne the same as chest acne?
Yes, back acne is the same as chest acne. Back acne refers to acne vulgaris that occurs on the back, while chest acne refers to acne vulgaris on the chest. Both types of acne are caused by factors such as genetics, hormonal fluctuations, and lifestyle habits, including poor diet and inadequate hygiene. Body acne is often linked to hygiene issues, including not showering after workouts, wearing tight clothing, and not washing clothes frequently. Back and chest acne can often be controlled with targeted skincare, topical prescriptions, oral medications, and in-office treatments.
Do steroids cause back acne?
Certain medications may increase your risk of developing Certain medications may raise your risk of developing back acne breakouts, including corticosteroids and anabolic steroids, both of which are sometimes shortened to “steroids.” Corticosteroids are a type of medication used to reduce inflammation in the body. They can be applied locally via injection, cream, or gel, or taken systemically through oral medication. Corticosteroids can stimulate the production of androgen hormones, potentially leading to increased sebum production. Anabolic steroids are synthetic versions of testosterone that promote muscle growth and development, as well as increase sebum production. With more sebum on the skin’s surface, the risk of clogged pores and back acne breakouts is higher.
Does back acne mean high testosterone?
While back acne isn’t directly caused by high testosterone, elevated testosterone levels can lead to back and facial acne. Hormonal shifts, which can occur anytime, are a major risk factor for developing back acne. Testosterone is a hormone found in both men and women, responsible for several health aspects, including bone density, sex drive, and fertility. Studies have shown that individuals with higher testosterone levels are more likely to experience acne breakouts. Excessive testosterone can stimulate increased sebum production, raising the risk of clogged pores and acne.
Can creatine cause back acne?
Creatine is a peptide that enhances athletic performance by accelerating muscle recovery and facilitating water retention within the body. Although the body naturally produces creatine, it can also be taken as a supplement, enabling athletes to train for longer periods. Currently, there is no known connection between creatine and acne breakouts. However, increased physical activity can cause more sweating, which may increase the risk of developing bacne. To prevent breakouts, people should wear breathable clothing during exercise and shower quickly afterward.
Will the sun help back acne?
Many patients believe that sun exposure helps clear acne, but in truth, the sun’s rays can dry out the skin, causing it to produce more oil to replace the lost moisture. Excessive oil production from overactive sebaceous glands can clog pores, leading to breakouts. UV rays can also cause serious skin damage, resulting in hyperpigmentation such as sun spots, age spots, melasma, and freckles, and can increase the risk of skin cancer.
Wearing sunscreen outdoors is essential for reducing the risk of bacne. Patients should choose a non-comedogenic, broad-spectrum sunscreen that they can apply regularly and consistently. A non-comedogenic skincare product means it won’t clog the pores. The sunscreen should also have a minimum SPF of 50 and be reapplied every 90 minutes when outdoors, with thorough washing off at the end of the day to maintain clear and acne-free skin. Dr. Green’s specialty skincare line, MGSKINLABS Inc., offers a non-comedogenic Hydrating Sunscreen with SPF 50 that also functions as a moisturizer. This type of sunscreen is ideal for individuals seeking to streamline their skincare routine, maintain healthy and moisturized skin, and protect against harmful UV rays that can lead to skin cancer and premature aging.
Will doxycycline treat back acne?
Yes! Doxycycline is an oral antibiotic with anti-inflammatory properties that can be prescribed to treat severe back acne breakouts. The medication kills the acne-causing bacteria present on the skin, thereby preventing breakouts. Oral antibiotics, such as doxycycline, should only be taken for a short period in small doses to avoid the development of antibiotic-resistant bacteria.
Does Spironolactone help with back acne?
Spironolactone is an oral medication used to treat hormonal acne in women by blocking androgens at sebaceous glands and reducing androgen secretion from the adrenal gland. Decreased androgen levels can reduce sebum production, resulting in fewer acne breakouts and flare-ups. The American Academy of Dermatology Association found that, on average, women notice a decrease in acne breakouts and oiliness in a few weeks while on Spironolactone.
Can you use tretinoin on back acne?
Tretinoin is a prescription retinoid often prescribed to treat acne. Retinoids and retinoid-like products, such as tretinoin, are a class of skincare products derived from vitamin A that work by exfoliating dead skin cells from the epidermis, the outermost layer of the skin. Dead skin cells, sebum, and debris are sloughed away at an increased rate, preventing the material from becoming trapped within the pores, which causes acne. Tretinoin can be prescribed by a board-certified dermatologist, such as Dr. Green, to help combat back acne and achieve clearer, smoother skin.

Does salicylic acid help with back acne?
Salicylic acid is a common ingredient found in acne skincare products. It helps promote your skin’s exfoliation by clearing pores of excess oil and dead skin cells. This acne-fighting ingredient appears in various skincare products, including cleansers, exfoliants, toners, and moisturizers. Using a salicylic acid cleanser or toner pad after working out is ideal to prevent sweat from clogging pores. The Pore Minimizing Cleanser and the Retexturizing Pads from MGSKINLABS both contain salicylic acid and glycolic acid to gently exfoliate the skin, helping prevent clogged pores and acne breakouts.
Does benzoyl peroxide help with back acne?
Ye ! Yes! Benzoyl peroxide is a highly effective ingredient for fighting acne, as it dries out active lesions, reduces inflammation, and kills the bacteria that cause acne. Benzoyl peroxide is found in certain face and body washes, as well as in spot treatments. MGSKINLABS’ Acne Spot Treatment contains 5% benzoyl peroxide to shrink and eliminate blemishes from the skin.
Do pimple patches work on back acne?
A pimple patch is an over-the-counter treatment designed to cover active acne lesions. Some patches contain hydrocolloid, a wound-healing ingredient that absorbs excess fluid and oil from whiteheads, forming a gel that is trapped in the bandage and kept away from the skin, causing the patch to turn white. Other patches are infused with chemical exfoliants, such as salicylic acid or glycolic acid, to kill acne-causing bacteria while gently exfoliating the skin. Pimple patches can be helpful because they prevent you from touching the acne, allowing it to heal properly and helping you resist the urge to pick or pop it. While pimple patches are effective for whiteheads, they tend to be less effective for cysts and blackheads. If you’re dealing with back acne, it’s important to see a board-certified dermatologist, like Dr. Green in NYC, who can help you understand the different types of lesions on your back and treat them most effectively.
How often should I shower with back acne?
Patients dealing with back acne should shower daily to prevent the buildup of dead skin cells, sebum, dirt, and other impurities on the skin. It is especially important to shower after exercising or heavy sweating to minimize the chance of sweat clogging the pores. Patients can use a salicylic acid or benzoyl peroxide cleanser in the shower to gently exfoliate the skin, reduce acne-causing bacteria on the surface, and help prevent back acne.

Can you get a tattoo with back acne?
According to tattoo artists and healthcare professionals, patients should wait to get a back tattoo until their back acne has cleared. Besides creating an uneven surface for the artist, tattooing over back acne can increase the risk of infection and spread acne bacteria from one area to another. If you are prone to back acne, seek treatment for it before scheduling any tattoo appointments.
Is body acne normal?
Yes, back acne is very common, affecting millions of individuals worldwide. Although acne isn’t a serious health issue, it can be frustrating and painful. Fortunately, many treatments are available to improve bacne. When dealing with any type of acne, the best first step is to consult a dermatologist, such as Dr. Green, for a personalized treatment plan. It is crucial to treat acne breakouts promptly to prevent the development of scars, which are often more difficult to treat than the initial breakouts. When you consult with Dr. Green on the Upper East Side of NYC, she will customize a treatment plan based on your specific back acne to help eliminate your acne for good and achieve clear, radiant skin.
Is back acne unattractive?
The presence of Back acne does not define attractiveness, but those experiencing it may feel self-conscious and less confident. Various treatments, including acne surgery, HydraFacials, VBeam laser, oral medications, and topical creams, can help manage and clear breakouts, restoring confidence. When you consult with expert board-certified dermatologist Dr. Michele Green in NYC, she will create a back acne treatment plan to help you look and feel your best again.
Why do back pimples hurt so much?
Back pimples can develop due to a genetic predisposition to increased sebum production or hormonal fluctuations that can increase sebum production. Often, back pimples arise from poor hygiene practices, including not showering after sweating or exercising, re-wearing clothes that are still damp, or wearing tight-fitting clothing. When dead skin cells, sweat, dirt, and sebum are trapped in pores, back pimples can develop. Bacteria can also become trapped in pores, resulting in inflammation and infection. These types of pustules, papules, and cysts on the skin can be painful due to the underlying inflammation. Treatment with topical or oral medications, or corticosteroid injections, can help shrink and eliminate the lesion, reducing any associated pain.
How to get started with back acne treatment today
Back acne is a skin condition that can be challenging to treat and may lead to feelings of self-consciousness and low self-esteem. Visiting a board-certified dermatologist as soon as back acne develops is crucial for preventing acne scars, which can be more challenging to treat than the breakouts themselves. If you’re struggling with back acne, various prevention strategies and treatment options are available, including acne surgery, HydraFacials, and VBeam laser, as well as oral and topical medications to help manage and treat breakouts. Scheduling a consultation with an acne expert, such as Dr. Michele Green in NYC, is the best way to understand and manage your breakouts, helping you achieve clear, acne-free skin.
Dr. Michele Green, in New York City, is an internationally renowned, board-certified dermatologist with over two and a half decades of experience providing customized acne scar and acne treatment plans to some of the world’s most discerning individuals. Taking a holistic approach to back acne treatment, Dr. Green will recommend a personalized combination of specially formulated skincare products, prescription treatments, and in-office therapies to help you achieve a healthy, clear, radiant, and pimple-free complexion that lasts. Dr. Green is recognized as one of the top dermatologists in New York City by Castle Connolly, Super Doctors, and New York Magazine for her dedication to patient care and expertise. To get started with eliminating your back acne once and for all, call 212-535-3088 or contact us online today to schedule a consultation with Dr. Green at her private dermatology office in Manhattan’s Upper East Side neighborhood.
 212-535-3088
212-535-3088